How to Improve Gut Health Naturally: The Ultimate Guide
Your gut microbiome influences everything from digestion and immunity to mood and skin health. This guide covers the science behind gut health and practical strategies to heal your microbiome naturally.
Author:
Victoria Samios, Microbiologist
Last Updated:
28 Nov 2025
Reading Time:
15 min
Categories:
Gut Health
how-to-improve-gut-health
What You'll Learn
This guide covers the science behind your gut microbiome and practical strategies to improve gut health naturally - from dietary changes and lifestyle modifications to understanding when professional testing might help.
Key Takeaways:
Your gut microbiome contains approximately 38 trillion microbes that influence everything from immunity and mood to skin health and weight
Simple dietary shifts (increasing fibre, reducing processed foods) can change your microbiome composition within 2-3 weeks
Common gut disruptors include antibiotics, processed foods, chlorinated water, and chronic stress
Signs of poor gut health extend beyond digestion - skin issues, mood changes, fatigue, and food sensitivities can all point to gut imbalances
Microbiome testing removes guesswork by showing exactly which bacteria are thriving or depleted in your gut
Why Is Gut Health So Important?
The past decade has seen a huge scientific effort to understand the gut microbiome. What researchers have discovered is remarkable: we are genetically more microbe than human. And by understanding our microbial inhabitants, we can change our gut health for the better.
One of the easiest approaches to naturally supporting your gut health lies not in what you do, but what you don't do. Choosing NOT to eat foods that encourage unfavourable microbes, or NOT following harmful lifestyle practices, is an important part of natural gut healing.
When you remove the obstacles, your microbial population can do the hard work for you - weeding out the troublemakers and restoring balance. The result? Better digestion, clearer skin, more stable energy, and improved mood.
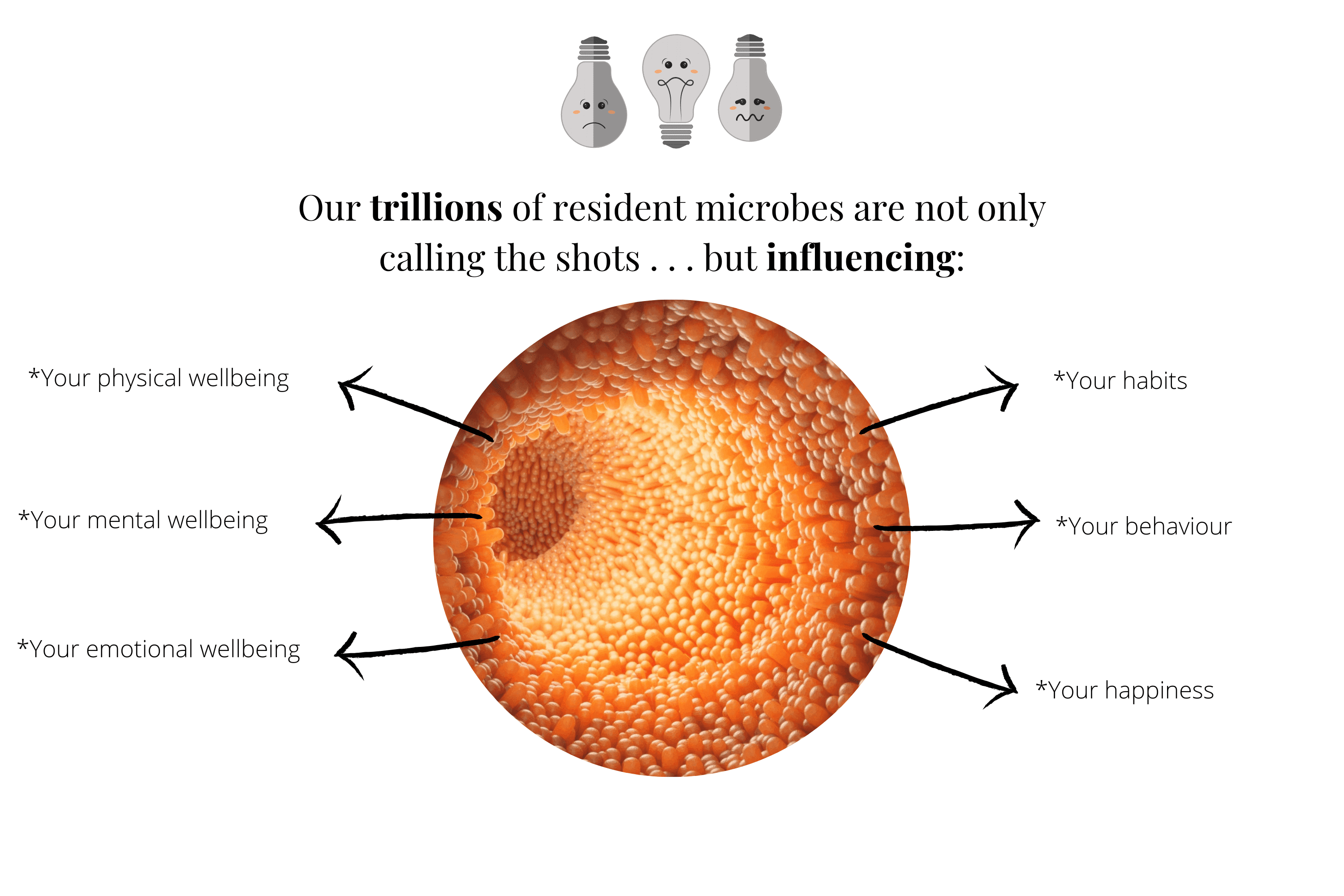
There is a huge and growing body of evidence suggesting your trillions of resident microbes are not only driving your physical health, mental and emotional wellbeing, but also influencing your habits, your behaviour, and your happiness.
The trillions of bacteria, fungi, and viruses living in your gut flourish within their own ecosystems. They create vitamins, metabolites, and energy not only for each other but symbiotically for you too—all without your conscious input.
The balance and diversity of your gut microbiome drive processes we traditionally believed were due to organ systems and cellular functions, including inflammation, immunity, and cellular integrity.
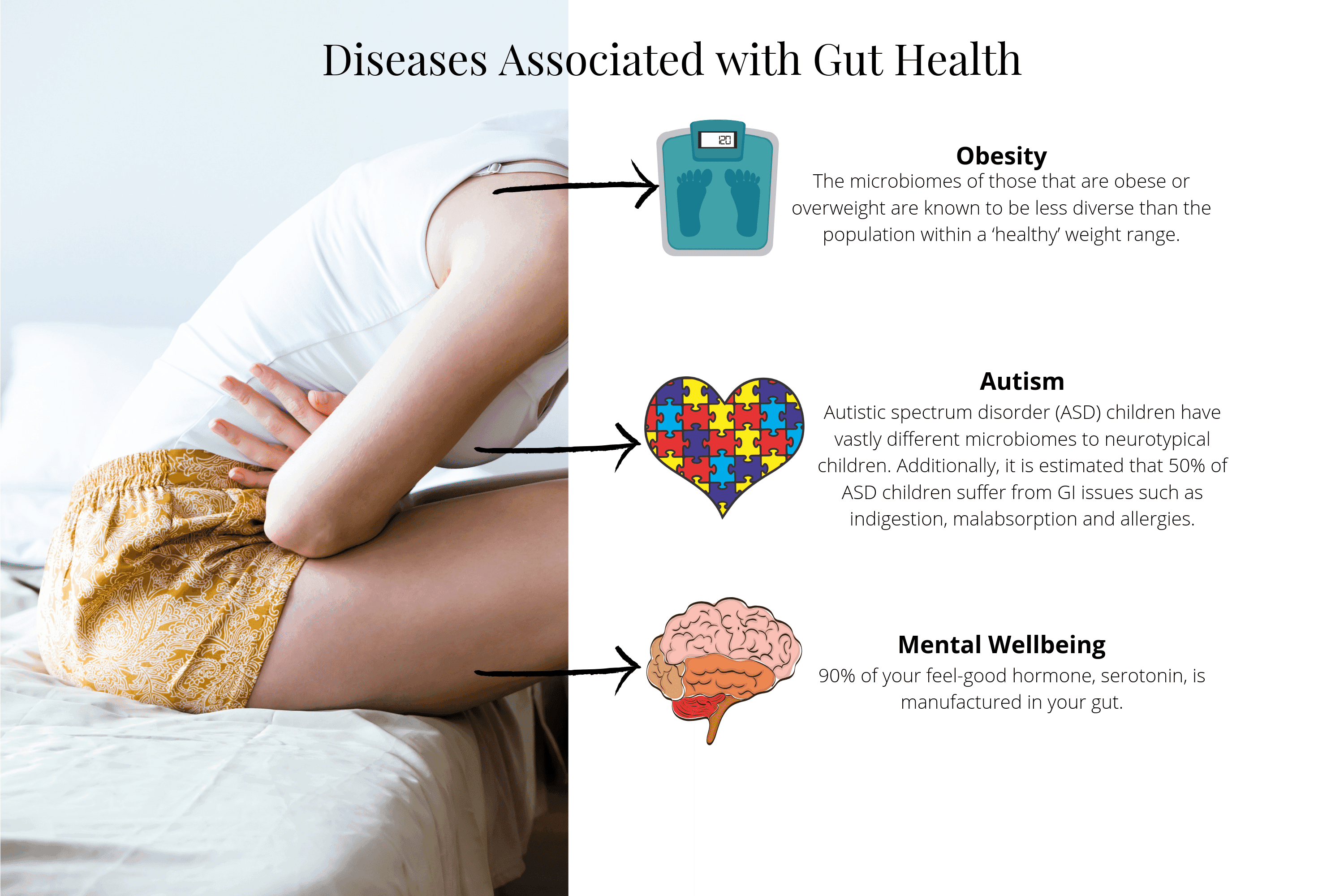
Diseases Associated with Gut Health
States of disease are increasingly being recognised as largely rooted in microbial pathways and managed by microbiome diversity, composition, and influence. This makes our daily choices far more important than we previously understood.
Obesity: The microbiomes of those who are obese or overweight are known to be less diverse than populations within a healthy weight range. Research shows that not only food and lifestyle choices play a crucial role in fat metabolism, but also gut bacteria. Animal studies support this—one study showed mice who received antibiotics in their first month of life developed 60% more fat than those not exposed to antimicrobial drugs.
Tip: Choose to avoid unnecessary antibiotic interventions to maintain microbial balance.
Autism: Children with autistic spectrum disorder (ASD) have vastly different microbiomes compared to neurotypical children. In a 2013 study, Italian researchers showed that ASD children's gut microbiota composition is very different from healthy children. The ecosystem of affected children is higher in unfavourable bacterial groups and produces vastly different metabolites. Additionally, it's estimated that 50% of ASD children suffer from GI issues such as indigestion, malabsorption, and allergies.
Tip: A microbiome test offers unparalleled insight into your microbiome, providing invaluable information to make appropriate choices for your family.
Mental Wellbeing: 90% of your feel-good hormone serotonin is manufactured in your gut. The interaction of microbes with specialised intestinal cells helps modulate the production of this critical hormone. Similarly, some bacteria themselves produce brain chemicals.
Tip: Happiness truly is an inside job. Learn more about the gut-brain connection and mood.
This all begs the question: which came first? Does an unhealthy microbiome develop as a result of disease, or do your dietary and lifestyle choices combine with your genetics to determine your microbiome?
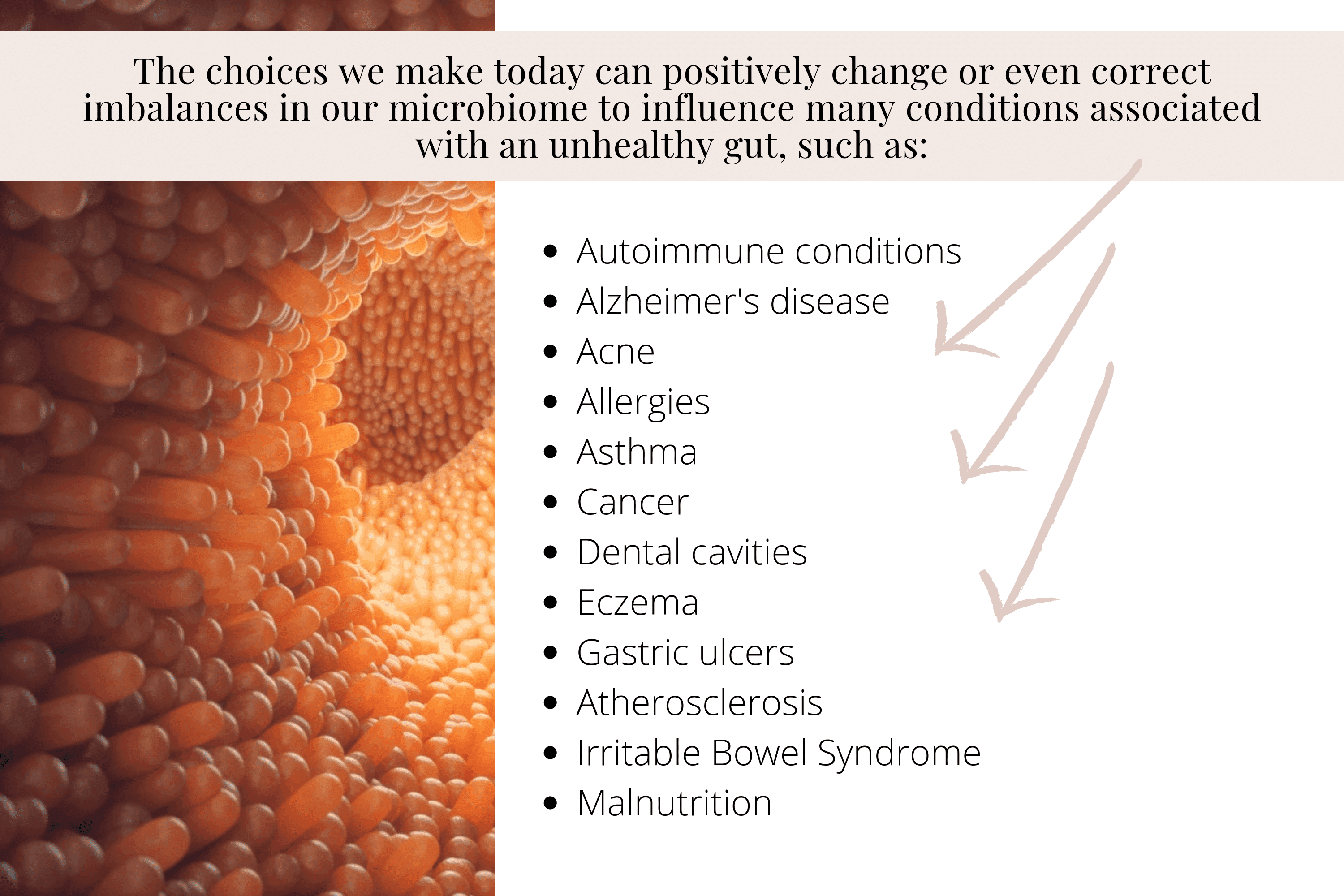
Research points to all of the above. The good news is that the choices we make today can positively change or even correct imbalances in our microbiome to influence many conditions associated with an unhealthy gut, including:
Autoimmune conditions
Alzheimer's disease
Acne
Allergies
Asthma
Cancer
Dental cavities
Eczema
Gastric ulcers
Atherosclerosis
Malnutrition
What Is Your Gut Microbiome?
Your gut, specifically your colon, is home to the largest concentration of microbes in your body. Current estimates suggest around 38 trillion microbes thrive in the 400g of material in your colon. Within this, your microbes make up approximately 200g.
When we talk about microbes, we describe all microbial life—not only bacteria. Like a rainforest is far more diverse than "just trees," our trillions of microbes are far more diverse than "just bacteria."
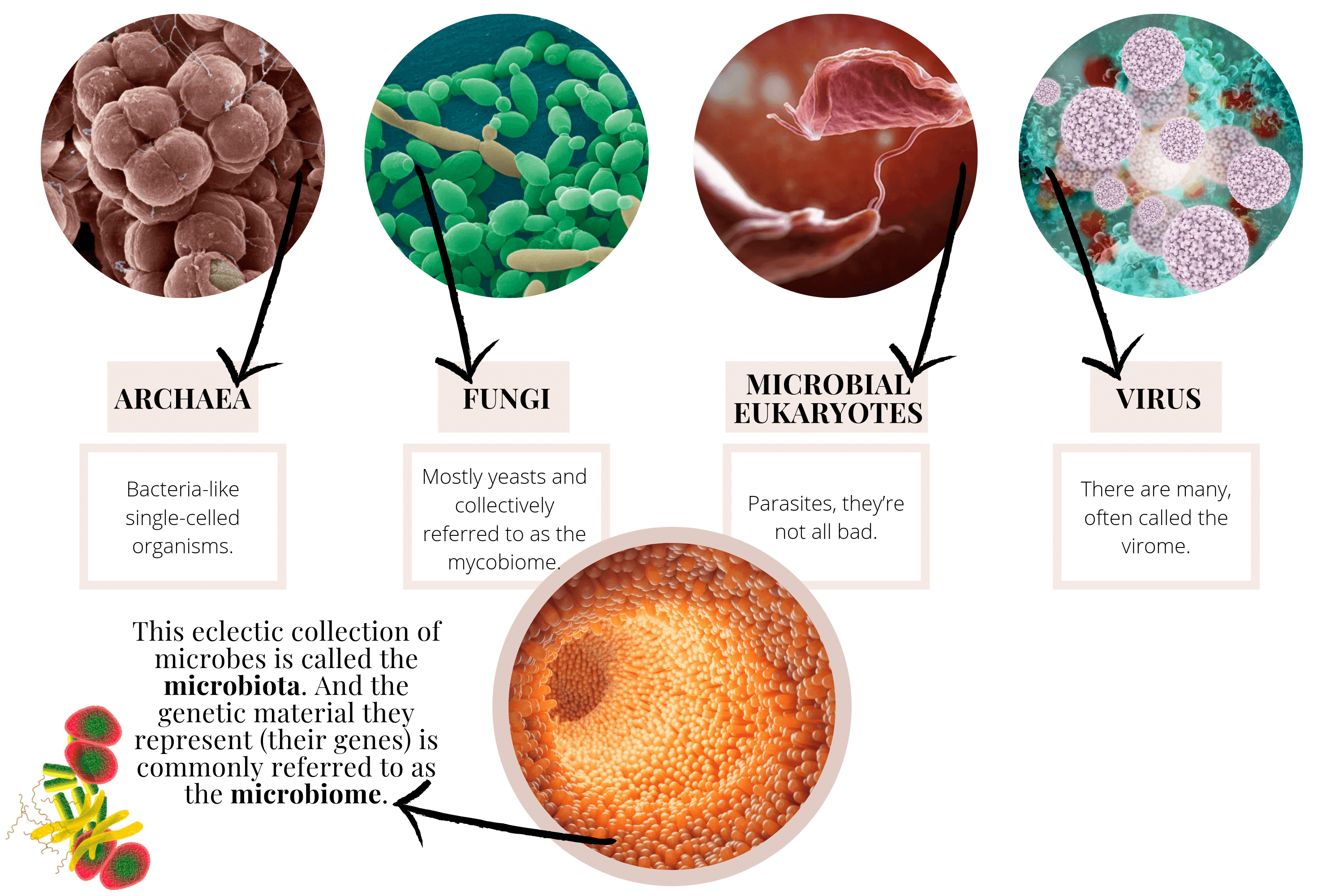
The scores of bacteria in your gut coexist with:
Archaea — Bacteria-like single-celled organisms
Fungi — Mostly yeasts, collectively referred to as the mycobiome
Microbial eukaryotes — Parasites (they're not all bad)
Viruses — Often called the virome
This eclectic collection of microbes is called the microbiota. The genetic material they represent (their genes) is commonly referred to as the microbiome.
In short, the gut microbiome is a 200g predominantly bacterial community (archaea, fungi, parasites, and viruses make up less than 0.1%) living in your large intestine, eating what you eat, and contributing a significant volume of DNA.
The most predominant gut bacteria fall into five phyla, although many others may be present:
Bacteroidetes
Firmicutes
Actinobacteria
Proteobacteria
Verrucomicrobia
As these large groups are examined further, the abundance of various bacterial genera and species are revealed. For example, the presence and abundance of Akkermansia muciniphila (a member of the Verrucomicrobia phylum) can be a positive finding as it plays a key role in maintaining gut integrity and mucus production.
Your gut microbiome reads like a menu of what you eat every day. Skilled practitioners can interpret microbiome test results to provide invaluable insight into not only what you eat but importantly what you don't eat—providing informed dietary recommendations and support on your healing journey.
Why Take a Gut Microbiome Test?
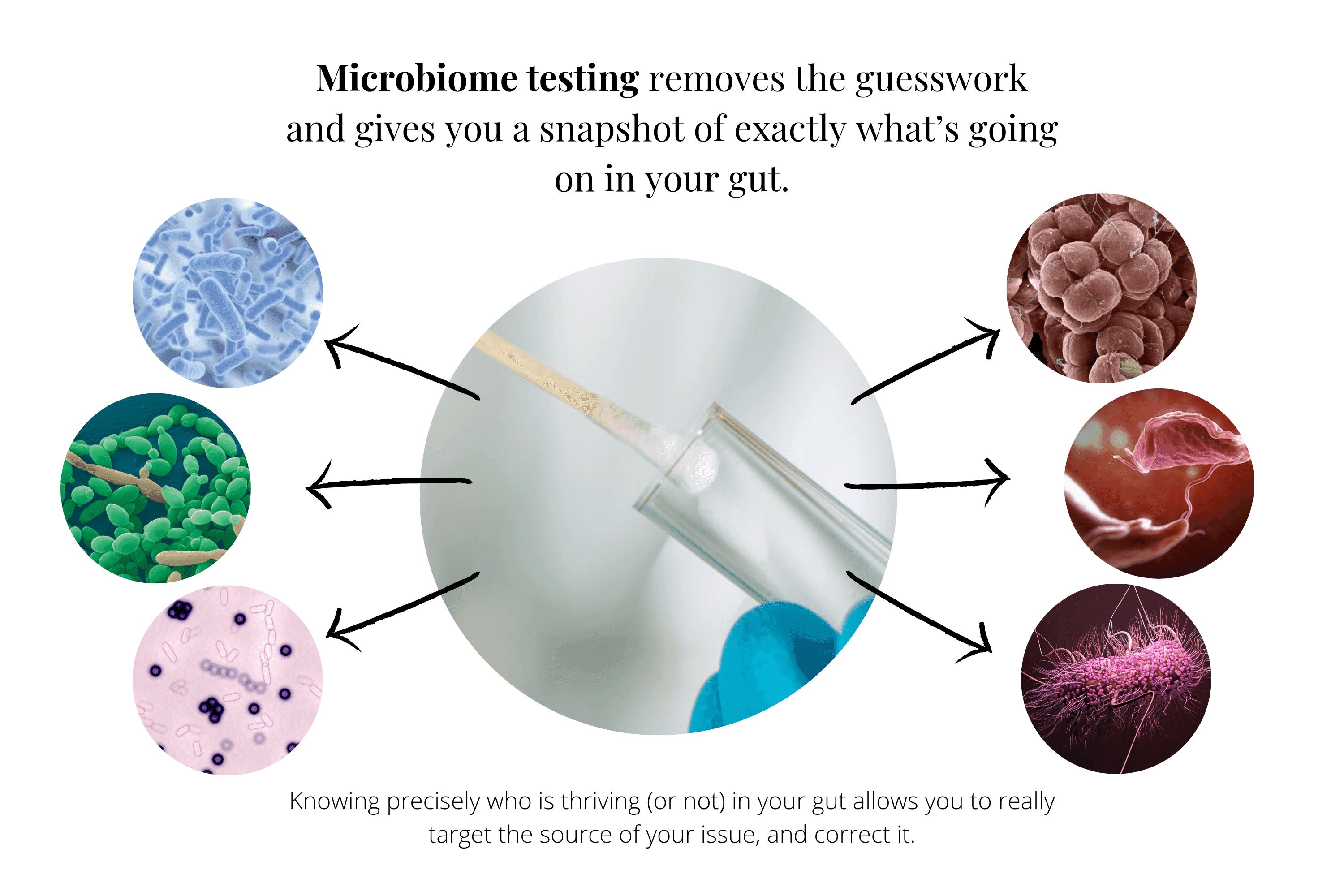
Knowledge is power. We know that different bacteria consume different foods and produce different by-products. Their relative abundance and balance can be controlled by you through diet.
You can choose who to feed.
Knowing precisely who is thriving (or not) in your gut allows you to target the source of your issue and correct it—quite the opposite of symptom spotting.
If you've been living with chronic health issues, you know how much energy can be spent finding someone who understands your individual health concerns. Microbiome testing removes the guesswork and gives you a snapshot of exactly what's going on in your gut.
Combined with appropriate dietary and lifestyle advice, microbiome testing can allow you to take back control of your health. It can change your life—and your resident microbes' too.
🔬 Not Sure What's Causing Your Gut Issues?
Comprehensive microbiome testing identifies the specific bacterial, fungal, or parasitic imbalances driving your symptoms - so you get answers, not guesswork.
Watch How Testing Works (2 min)
Book Your Free Evaluation Call
Gut Health and Your Body
One of the most empowering outcomes of microbiome awareness is rooted in the intrinsic ability of the body to heal.
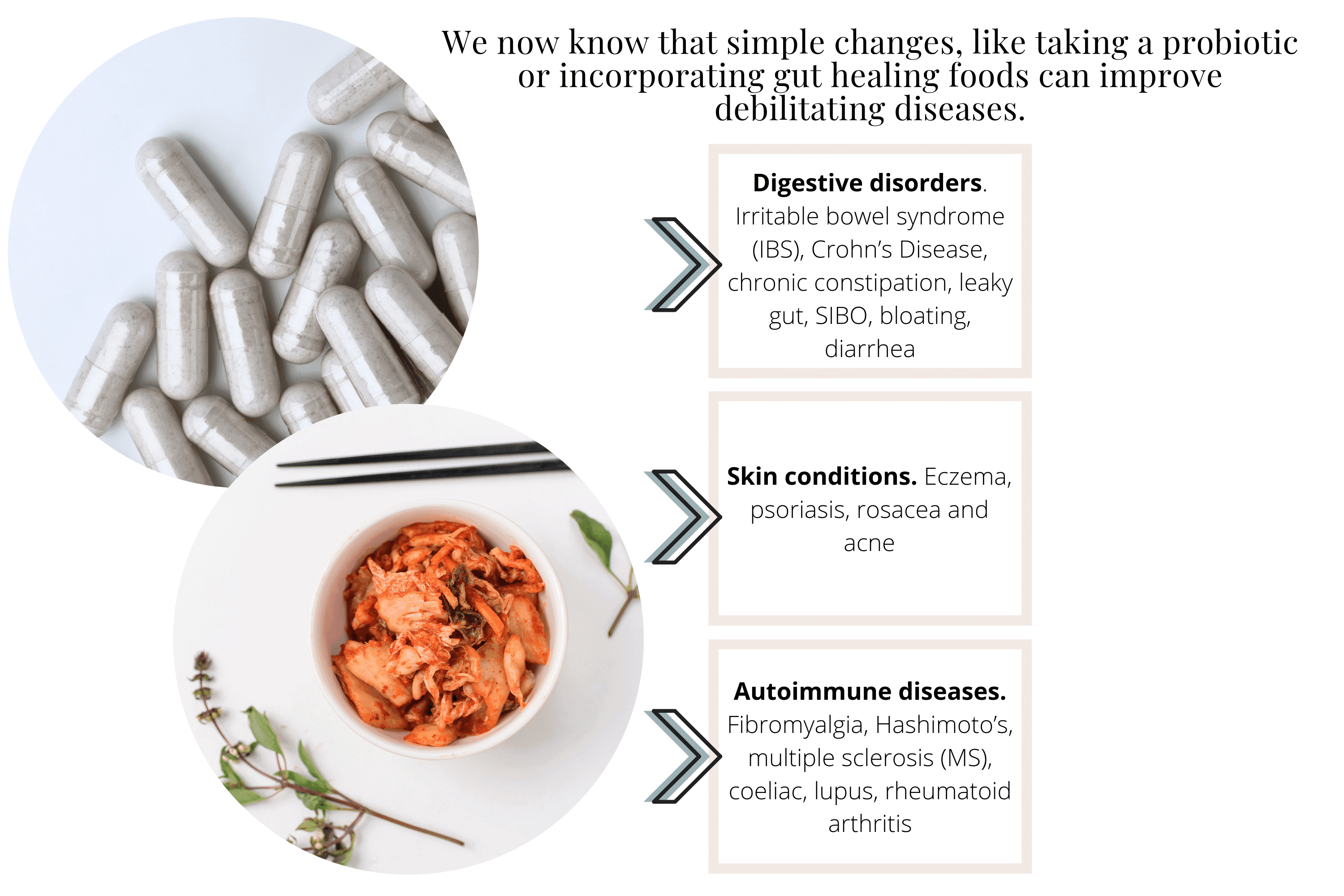
We now know that simple changes—like taking a targeted probiotic or incorporating gut healing foods—can improve debilitating conditions including:
Digestive disorders: Irritable bowel syndrome (IBS), Crohn's disease, chronic constipation, leaky gut, SIBO, bloating, diarrhoea
Skin conditions: Eczema, psoriasis, rosacea, acne
Autoimmune diseases: Fibromyalgia, Hashimoto's, multiple sclerosis, coeliac, lupus, rheumatoid arthritis
As you begin to understand how your digestion and microbes work, you'll begin to make choices based on their wellbeing—which will, in turn, influence your own.
We are a superorganism. A collection of many, all with a common goal. Our bodies do not set out to work against us (although it may feel like it at times). Our bodies want to be well, and disease is simply a symptom of an imbalance—a call for help.
Understanding the source of our symptoms is the key to wellbeing. When we remove foods and practices that harm us, our body and our microbes restore balance. That innate intelligence within all life works towards health.
The microbiome adjusts. The body heals. And the mind comes along for the ride.
Gut Health and Your Mind
We are fortunate to witness the growing research linking gut health to mental health.
It is now common knowledge that the gut is home to millions of neurons and produces neurotransmitters—messengers for sending and receiving messages to AND from the brain.
It's little wonder we use phrases like "gut feeling," "gut instinct," and "food for thought," describing this connection long before science discovered it.
People all over the world are healing from mental health challenges through diet, with the right support and lifestyle changes. New fields are emerging like nutritional psychiatry, exploring the gut-brain connection and finally acknowledging that food can treat psychological conditions.
It was never "all in your head."

The Gut-Brain Connection
It is also in your gut.
The gut is home to your Enteric Nervous System (ENS)—an intricate network of neurons deeply connected with your gastrointestinal tract. This includes the vagus nerve, the largest pathway connecting your brain to your gut. And it's a two-way street: signals go both ways.
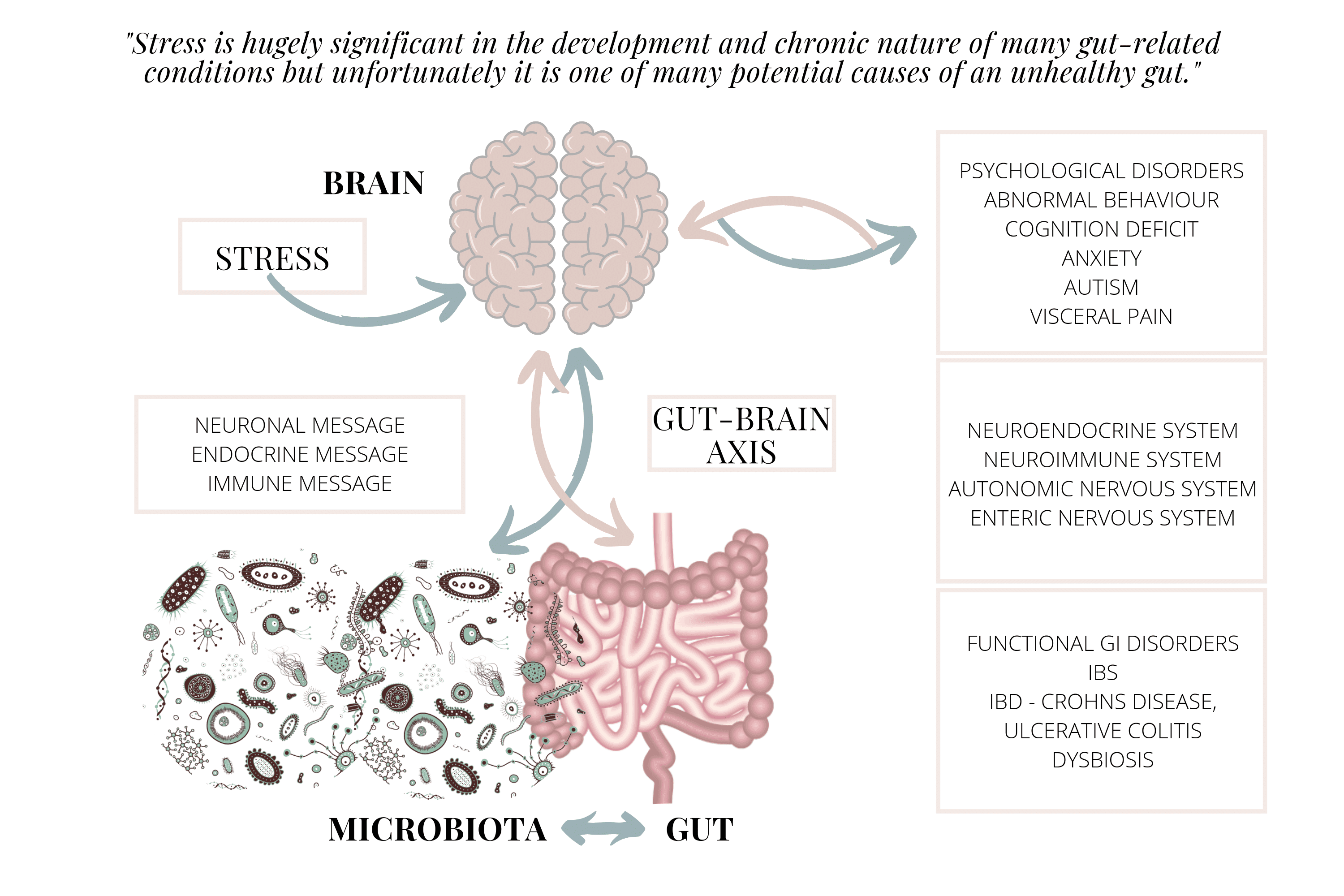
Not surprisingly, stress has been found to inhibit the vagal nerve and has negative effects on the GI tract and microbiota. Stress is involved in the disease processes of many illnesses, including IBS and IBD (inflammatory bowel disease).
The role of stress in disease is widespread, and stress reduction is an important consideration for everyone—especially those looking to heal gut issues.
Stress is hugely significant in the development and chronic nature of many gut-related conditions. Unfortunately, it is one of many potential causes of an unhealthy gut.
What Causes an Unhealthy Gut
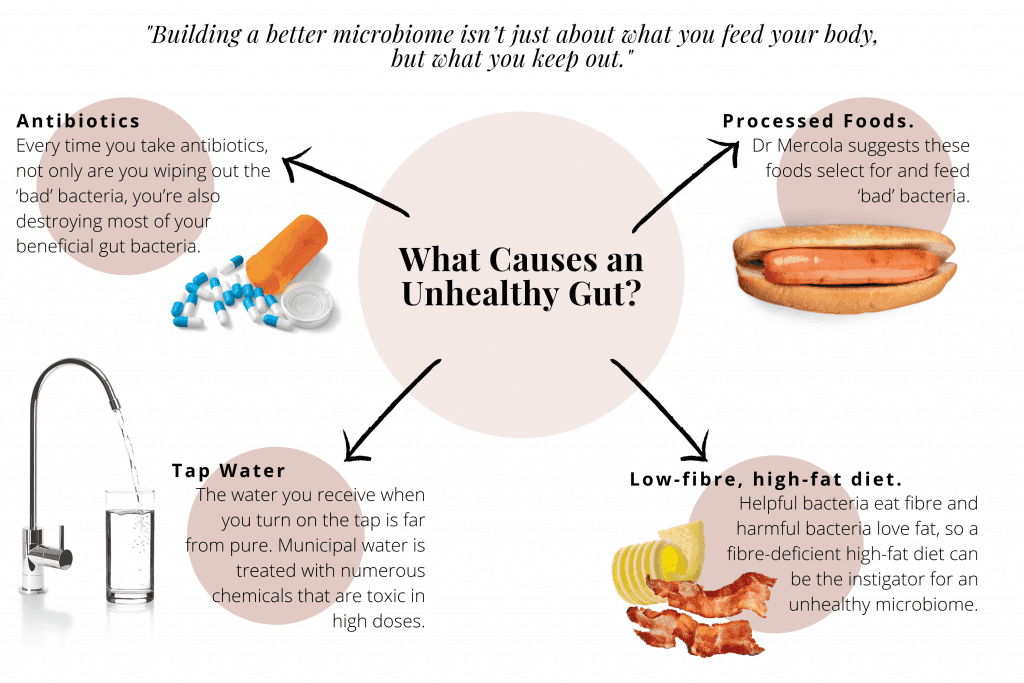
Building a better microbiome isn't just about what you feed your body, but what you keep out. Modern life has introduced many microbiome polluters—substances that critically change the composition of your microbiome.
Sadly, they are often hidden in your daily routine. If you're looking for an easy place to start with gut healing, eliminating microbiome polluters is an excellent first step.
Antibiotics
Antibiotics have been designed to be anti-biotic—meaning against living organisms. Rather than being targeted, they are wide-acting chemicals whose effects have been likened to a "bomb going off" in your gut.
Antibiotics undeniably save lives but should be used only when absolutely necessary. Every time you take antibiotics, you're not only wiping out the "bad" bacteria—you're also destroying most of your beneficial gut bacteria. It can take years for your body to rebalance without additional help.
Tip: Supplementing with a high-quality probiotic and eating fermented foods after taking antibiotics will help reseed and support your microbiome balance.
Processed Foods
Ultra-processed foods common in the Western diet are a relatively recent addition to the human menu. They're often high in refined carbohydrates and harmful sugars while devoid of any real nutritional benefit.
Diets rich in these food-like substances don't support the beneficial bacteria that the human pre-fast-food diet nurtured. These foods select for and feed unfavourable bacteria. Additionally, many artificial additives found in processed foods, like Polysorbate 80, have a detrimental effect on your microbiome.
Tip: If it's in a packet and you can't pronounce it, don't eat it.
Tap Water
The water you receive when you turn on the tap is far from pure. Although it may be free of bacterial and protozoan infectious organisms due to heavy chlorination, it contains a multitude of other substances.
Municipal water is treated with numerous chemicals. The Australian Drinking Water Guidelines describes buffering agents used in addition to the well-known chlorine and fluoride. Some of these chemicals mimic important thyroid hormones—substances collectively termed endocrine disruptors.
Tip: Use water filters in your kitchen and install a shower filter to reduce your family's exposure. Heated water increases both vaporisation of chemicals and your skin's permeability.
Low-Fibre, High-Fat Diet
Low-carb diets are popular right now, with bacon and butter being promoted as health foods. In moderation, these foods can be a balanced part of any diet. However, problems arise when we prioritise fat and reduce health-supportive fibres.
Helpful bacteria eat fibre, and harmful bacteria love fat. A fibre-deficient, high-fat diet can be the instigator for an unhealthy microbiome.
Tip: Take Michael Pollan's sage advice: "Eat food. Not too much. Mostly plants." And you'll be well on your way to getting enough fibre—think soluble, insoluble, and resistant starch.
Gut Microbiome Case Study
An intriguing case study into the effects of a pre-modern-era diet was conducted by Jeff Leach, an anthropologist studying the microbiomes of the Hadza—a central Tanzanian hunter-gatherer tribe whose existence has remained largely unchanged for 10,000 years.
No antibiotics, no processed anything (they don't even cultivate crops), seasonal rainwater, and a very primal high-fibre diet.
He mapped his own microbiome on both the Standard American Diet (with the apt acronym SAD) and after following the Hadza fibre-rich diet.
[IMAGE: Hadza Diet Microbiome Comparison Graph (existing file: Gut-bacteria-image-graph.gif)]
The results show a striking shift in the predominance of Firmicutes (a fat-loving phylum known to contribute to obesity) and Bacteroidetes (a phylum associated with leanness and overall health).
On the left, the SAD diet results are dominated by the red-coloured Firmicutes. The graph on the right shows a dramatic shift to the blue-coloured Bacteroidetes flourishing in response to his increased consumption of fibre—only 2-3 weeks later.
This illustrates both the importance of microbiome testing and the rapid response of the microbiome. Bacteria replicate in response to food availability and decrease in response to food scarcity—exponentially.
It's the balance of health-promoting microbes and less favourable species that determines how you feel and how your body responds to their metabolites.
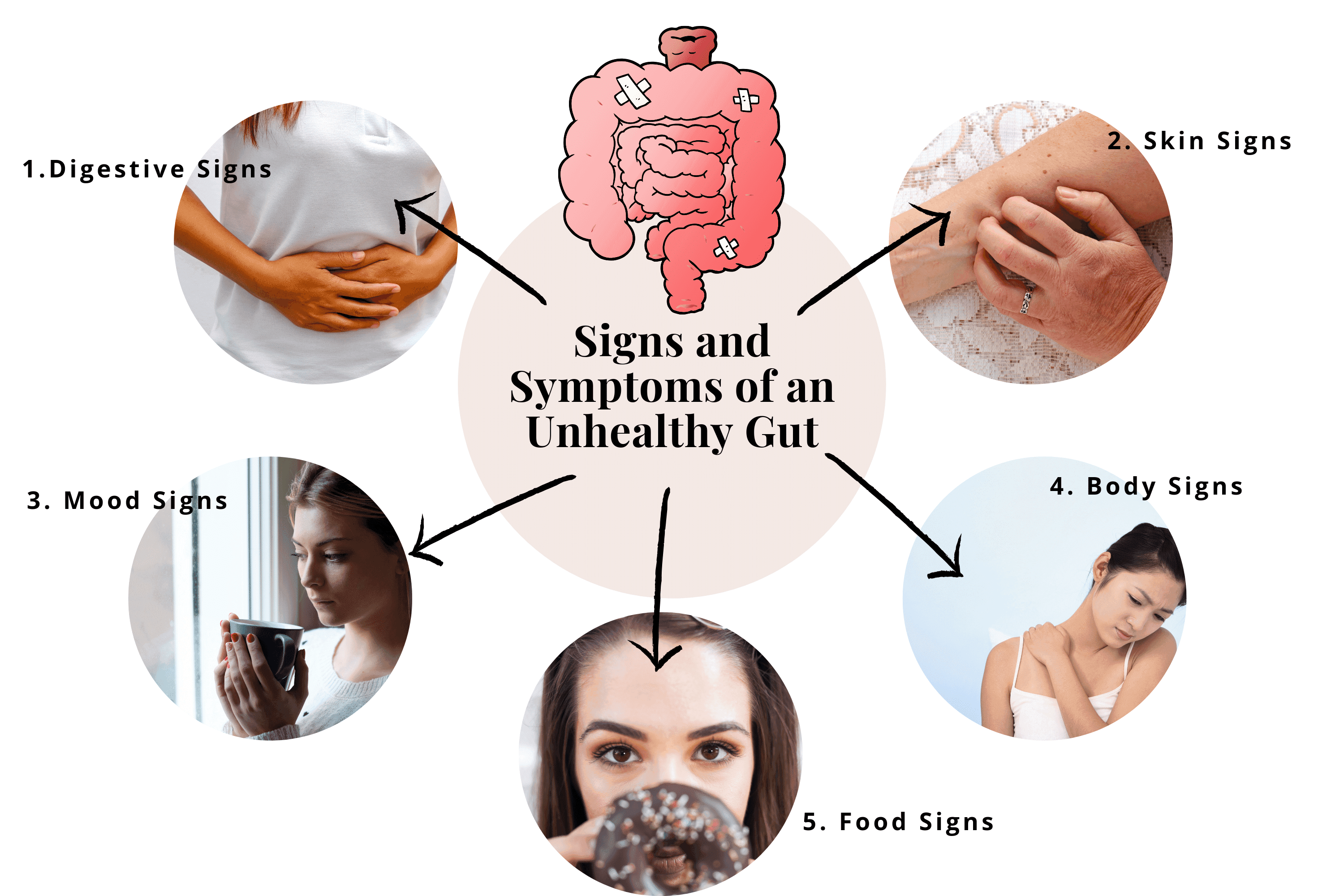
Signs and Symptoms of an Unhealthy Gut
We often don't realise how unwell we were until we feel better. The discomfort becomes a constant companion and our frame of reference. We learn to tolerate and live with all the niggly symptoms of disturbed health.
We miss the signs. It's only when we look back that we see how far we've come.
If you're struggling with one or more of the following symptoms, gut microbiome testing might be helpful for you.
Digestive Signs
Typical upset stomach symptoms like chronic diarrhoea, constipation, bloating, and flatulence can all point to an unbalanced microbiome or dysbiosis. These can be caused by bacterial, fungal, or parasitic disturbances resulting in inflammation, excessive gas production, irritation, or leaky gut. Other symptoms include bad breath and heartburn.
Skin Signs
Our skin is said to be a mirror of our gut. Dark circles under the eyes, acne, blotches, rashes, and rosacea can all be associated with gut troubles. Eczema—a chronic inflammatory skin condition—is particularly noteworthy. Elimination diets can be very effective for relieving skin conditions as they are easily visually monitored.
Mood Signs
Significant mood changes can indicate poor gut health. Seemingly harmless symptoms like moodiness, headaches, and brain fog can be the beginning of more concerning symptoms like anxiety, depression, and memory loss. ADD, ADHD, and other behavioural and psychological syndromes have been shown to respond favourably to improvements in gut health.
Body Signs
Your body will try to alert you to hidden gut issues with symptoms such as sleep disturbances, rapid weight change, and fatigue. More serious symptoms like autoimmune conditions (lupus, rheumatoid arthritis, Crohn's disease, coeliac) are also heavily involved in unhealthy gut processes. Low immunity, joint pain, or arthritis can also point to the gut.
Food Signs
If you battle with food cravings or food intolerances and sensitivities, chances are your gut is the culprit. Eating a diet high in sugar or suffering with nutritional deficiencies are also indicators of a gut out of balance.
Important: If you suffer any of the symptoms mentioned above, it's important to get assessed by your healthcare provider or a qualified practitioner. While these symptoms are typical of gut health issues and related conditions, there may be other underlying causes.
📋 Recognise These Symptoms?
If you've been struggling with gut issues for months without answers, comprehensive testing can identify exactly what's driving your symptoms.
Book Your Free Evaluation Call
How Foods Help or Hurt Your Gut
Diet is the most natural and empowering way to address your gut health. Choosing to eat foods that positively influence your microbiome and avoid those that don't is a crucial step in gut healing.
There are a growing number of diets that have had wonderful results for people all over the world: Paleo, Keto, Plant-Based Whole Food, Low-Carb High-Fat, Gluten-Free Casein-Free, and everything in between.
While all this information is wonderful, the conflicting advice can quickly become overwhelming. This is why working with a qualified practitioner who has tested your microbiome can fast-track your healing and take the guesswork out of choosing the right diet for you.
In the meantime, understanding how food affects your gut is an important step forward. Often, simply eliminating troublesome foods will produce noticeable improvements.
How Wheat Affects Your Gut
Wheat has received a lot of attention recently, and with good reason. In addition to heavy spraying and ever-increasing glyphosate concentrations, modern-day wheat is very high in gluten.
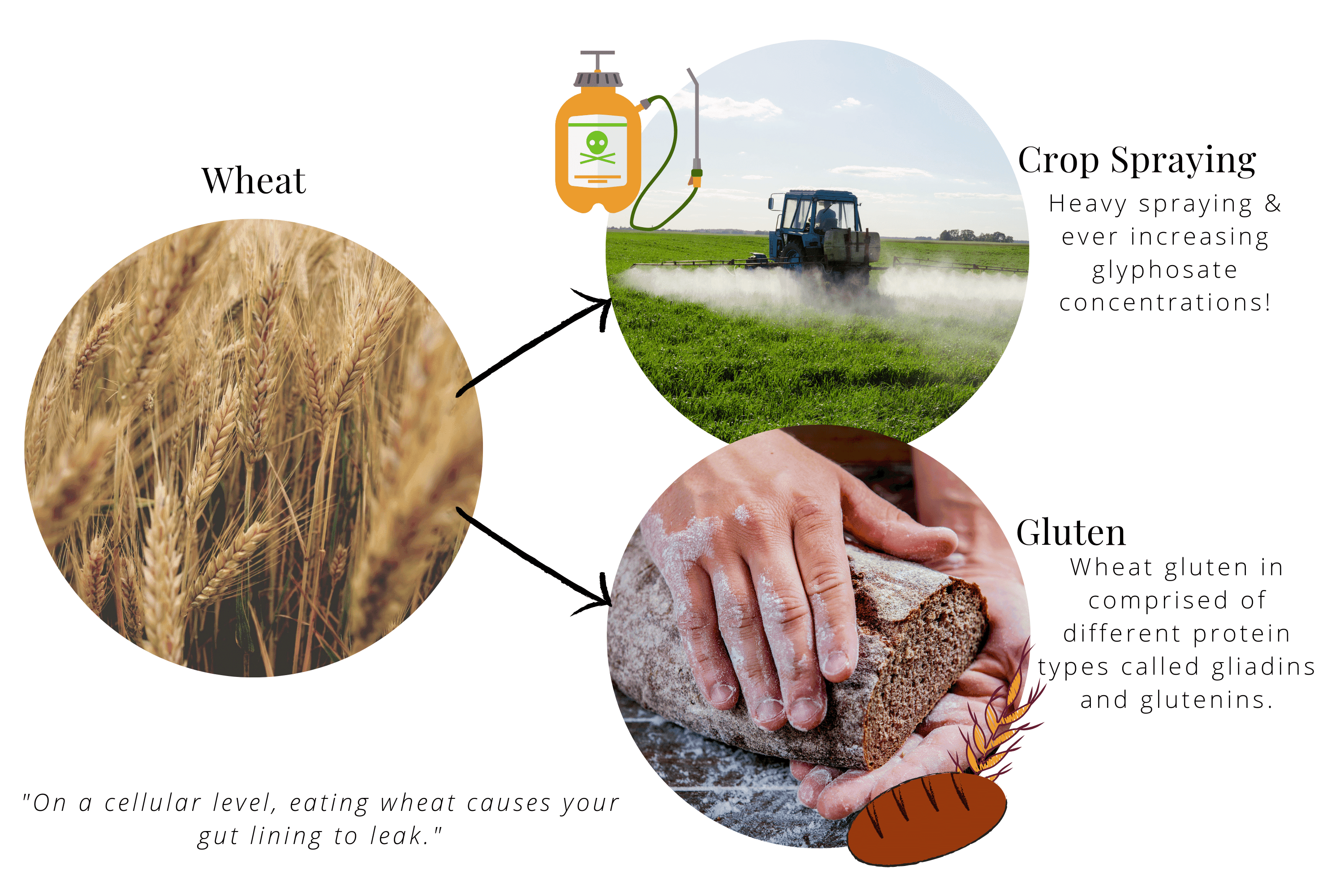
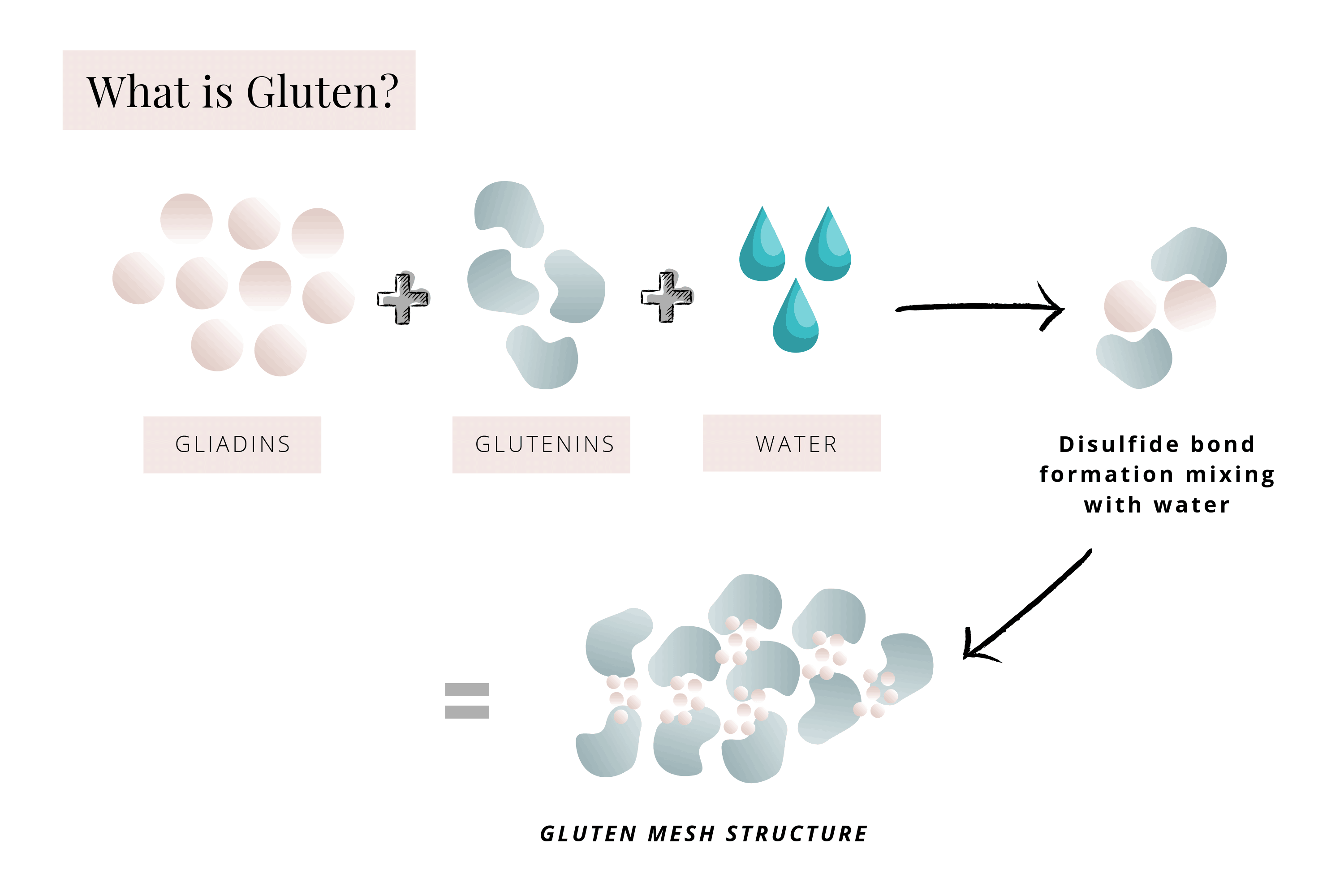
Wheat gluten is comprised of different protein types called gliadins and glutenins. These soluble gliadin proteins act as messengers, triggering your gut lining cells to produce and release another protein called zonulin, which opens the spaces between gut cells (called tight junctions).
This increased permeability allows large molecules, including gluten, to pass through the gut lining, causing an inflammation cascade of immune cells, cytokines, and symptoms of what is commonly referred to as leaky gut.
On a cellular level, eating wheat causes your gut lining to leak.
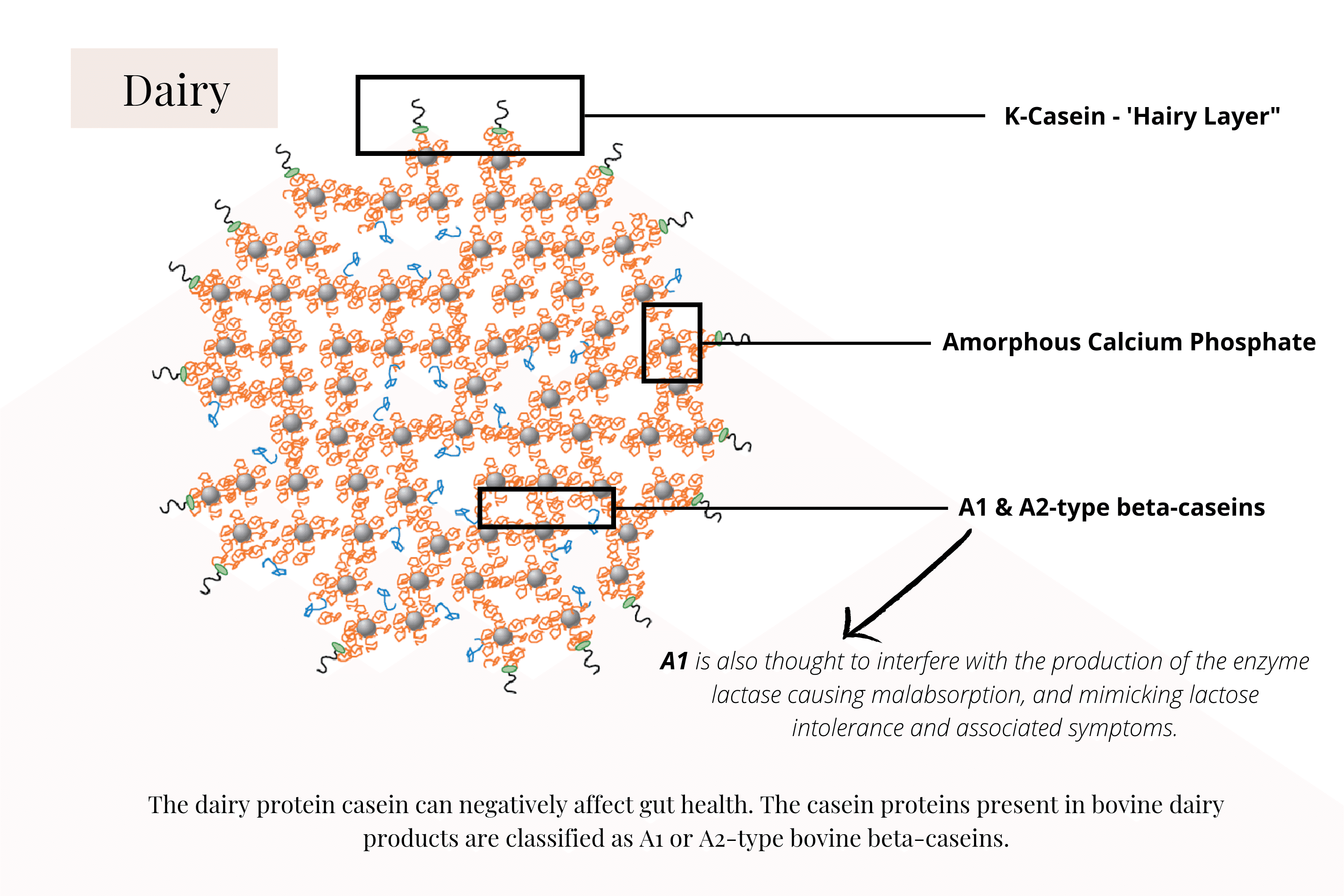
What Dairy Does in Your Gut
Similarly, the dairy protein casein can negatively affect gut health. The casein proteins present in bovine dairy products are classified as A1 or A2-type bovine beta-caseins.
A1 caseins have been shown to stimulate gastrointestinal inflammation by releasing the opioid beta-casomorphin. A1 is also thought to interfere with the production of the enzyme lactase, causing malabsorption and mimicking lactose intolerance and associated symptoms.
Other troublesome and common foods include soy, refined sugar, caffeine, and alcohol.
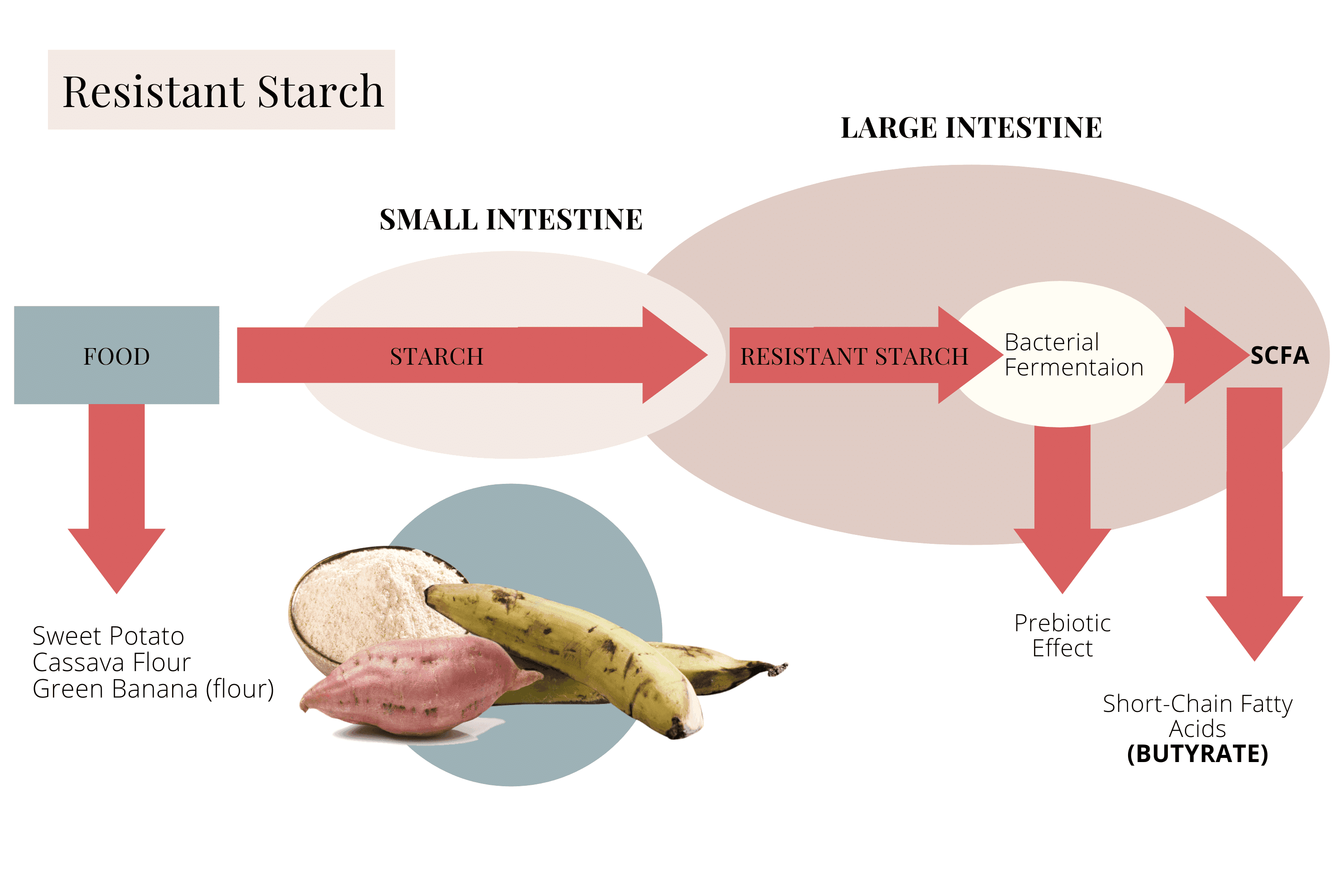
The Resistant Starch Pathways in Your Gut
On the other hand, consuming foods rich in resistant starch helps nourish and heal the gut. When resistant starch reaches the large intestine intact, it feeds bacteria that produce short-chain fatty acids (SCFAs).
Butyrate is one of these SCFAs and has been associated with many health benefits, including reduced intestinal inflammation, increased cellular fluid transport, increased motility, and reinforced gut cell defences.
All very good reasons to eat more foods rich in resistant starch.
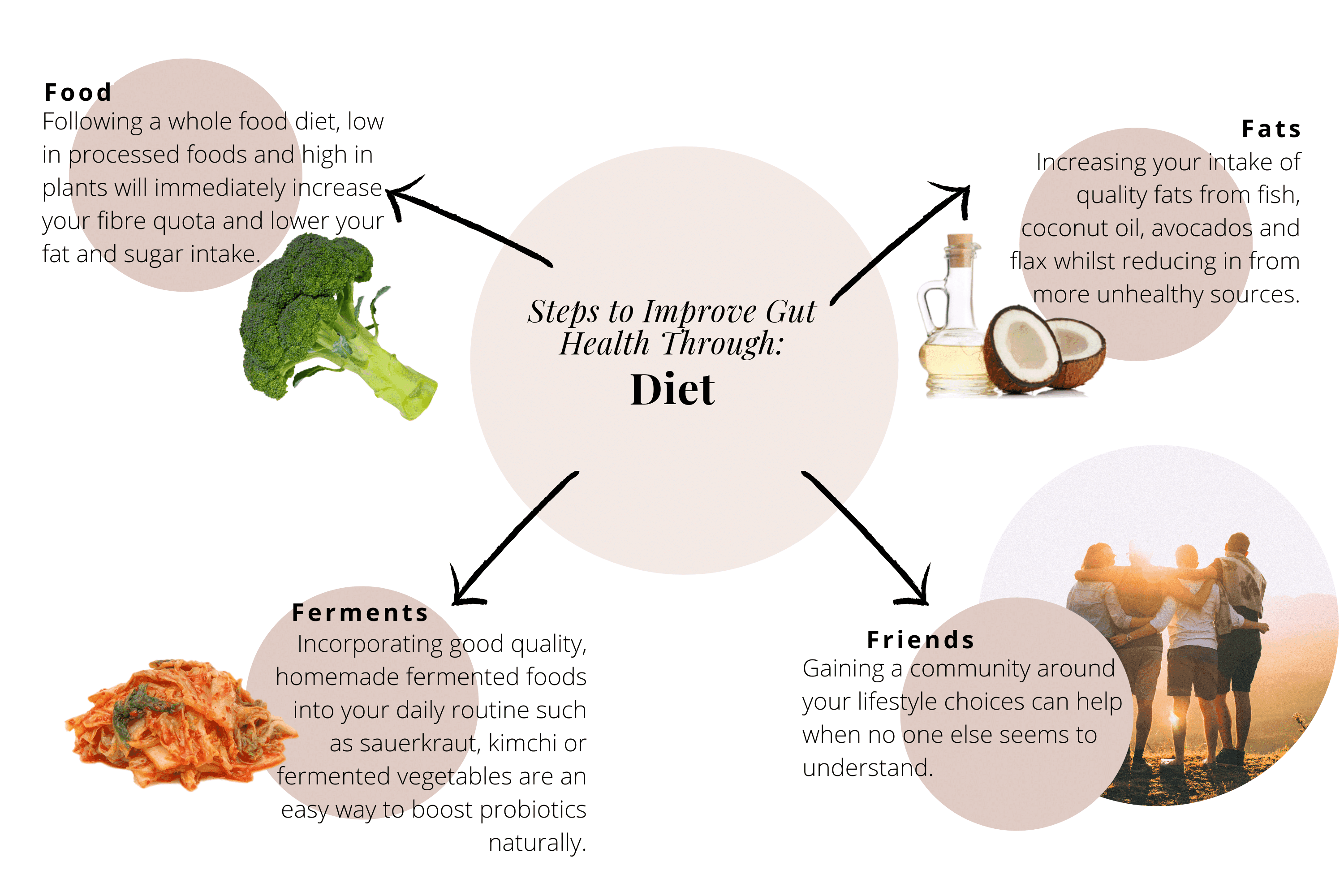
Steps to Improve Gut Health Through Diet
While these are broad guidelines for improving gut health through diet, it's important to remember that your microbiome is unique. It's a complex fingerprint of all the foods, experiences, and life that has gone before you.
What works for someone else may not work for you. You need to tune into your body, understand what's in your microbiome, and go from there—gently.
Some widely regarded starting steps include:
Food
Following a whole food diet low in processed foods and high in plants will immediately increase your fibre quota (to feed your helpful microbes) and lower your fat and sugar intake. Keeping stalks on fibrous vegetables like broccoli, cauliflower, and asparagus are instant resistant starch boosters. Leeks are also wonderfully fibre-full.
Further reading: 26 Best Foods for Gut Health
Fats
Increasing your intake of quality fats from fish, coconut oil, avocados, and flax whilst reducing unhealthy sources such as vegetable oils and excessive saturated fats will help heal and repair your gut lining.
Find out more: Gut Bacteria and Weight Loss: The Surprising Connection
Ferments
Incorporating good quality, homemade fermented foods into your daily routine—such as sauerkraut, kimchi, or fermented vegetables—is an easy and cost-effective way to boost probiotics naturally. A tablespoon a day can be enough to keep unfavourable microbes at bay.
Probiotics
The importance of good bacterial friends cannot be emphasised enough. Consider adding a reputable multi-strain, high-CFU probiotic to support your microbiome while making dietary changes.
Learning to listen to your body and monitor how it responds to diet and lifestyle changes is a powerful gut-healing practice and important life skill.
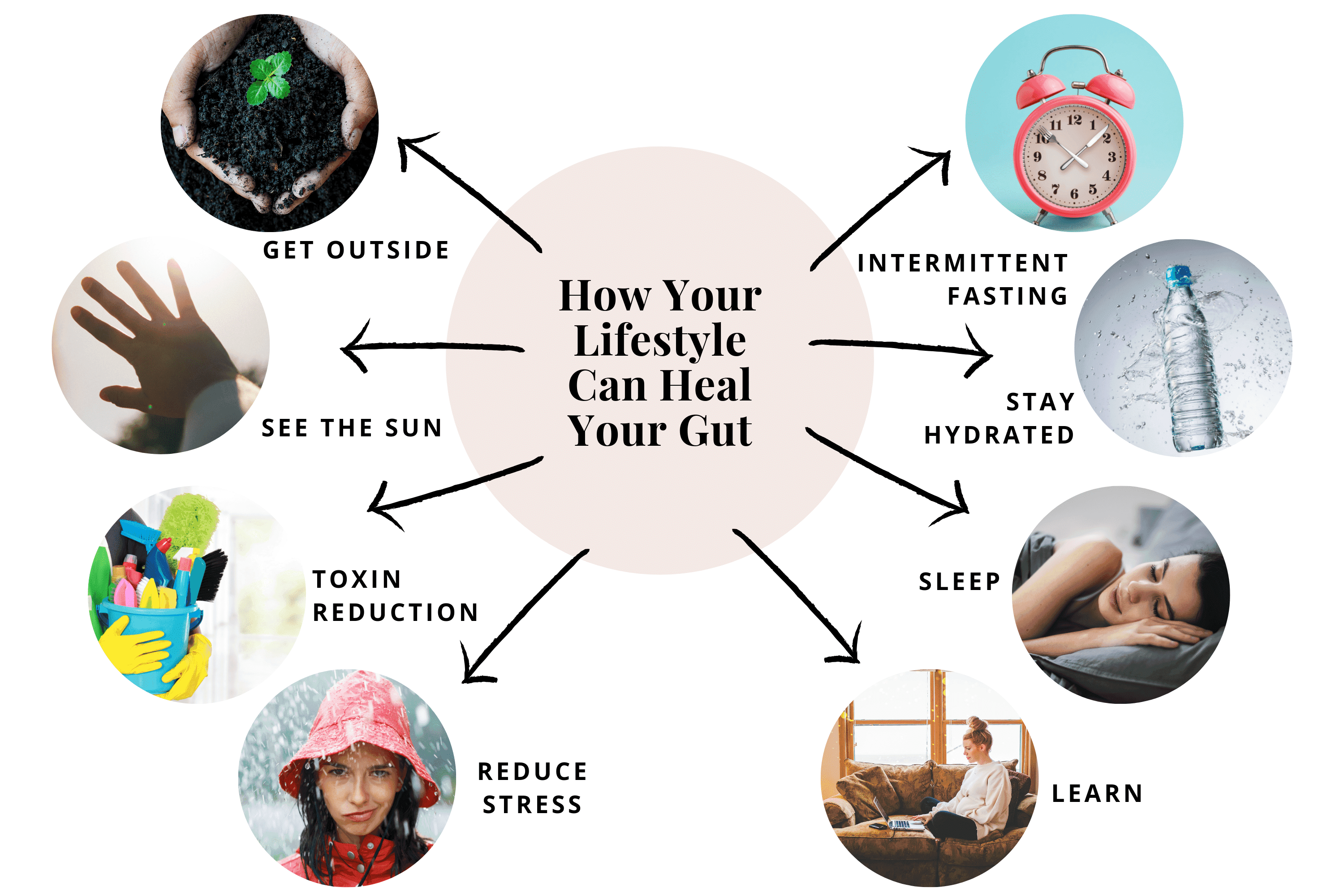
How Your Lifestyle Can Heal Your Gut
In addition to feeding your microbiome for health, there are a number of gut-supportive lifestyle choices you can incorporate into your week.
Get Outside
Numerous studies have linked dirt microbes to better gut health. Mycobacterium vaccae found in soil has been shown to fight depression and boost immune responses. While M. vaccae can be bought as a probiotic, it lives free of charge in your garden. So forget the hand sanitiser and get dirty.
See the Sun
While sunlight is undeniably good for mental wellbeing, vitamin D deficiency has been shown to reduce antimicrobial molecules (defensins) that are important for maintaining healthy gut flora.
Toxin Reduction
Reducing your exposure to xenobiotic chemicals and pesticides will help you maintain your microbiome diversity. Commonly used chemicals such as chlorine, sanitisers, and household insecticides are designed to kill microorganisms—including yours.
Reduce Stress
Stress comes in many forms: psychological stress, sleep disturbance, environmental stressors, diet, physical activity, noise, and even pollutants. Research shows that stress impacts the function, composition, and metabolic activity of the gut microbiome.
Intermittent Fasting
Fasting is quickly becoming a recognised beneficial practice for improving and maintaining gut health. Intermittent fasting involves eating and fasting in cyclical patterns, often with up to 18 hours between meals. The health benefits are proving to be highly popular.
Stay Hydrated
Keeping you and your gut microbes well watered is an easy way to maintain a healthy gut naturally. Around 8 litres of water per day is absorbed in digestive processes. Make sure your water is as pure as possible.
Sleep
Sleep has long been touted as a cure-all, and conversely, sleep deprivation has serious consequences. Your microbiome plays a crucial role via the gut-brain axis and also directly.
Serotonin and GABA are important neurotransmitters involved in relaxation and sleep—both are produced by gut bacteria. Streptococcus and Enterococcus produce serotonin, which helps make the sleep molecule melatonin. Lactobacillus and Bifidobacteria produce GABA, which decreases beta-brainwaves and increases calming alpha-brainwaves.
Learn
One of the most empowering things you can do for your family's health is educate them on the importance of gut health. Incorporating simple diet and lifestyle changes into your everyday routine can reap massive physical, emotional, and environmental benefits.