Candida Overgrowth: Real Concern or Overstated Problem?
Author:
Amanda Ledwith, BHSc Naturopathy
Last Updated:
23 Jan 2026
Reading Time:
8 mins
Categories:
Gut Health
candida-overgrowth
What You'll Learn
Candida is a fungus that naturally lives in the gut, mouth, and vagina. While genuine Candida overgrowth can contribute to gut permeability, inflammation, and systemic symptoms, it's often over-attributed as a root cause when other factors—bacterial dysbiosis, SIBO, or general gut imbalance—are actually driving symptoms.
Many people spend years treating "Candida" based on symptom checklists without ever confirming whether fungal overgrowth is actually present. Comprehensive metagenomic testing can detect true Candida elevation alongside the bacterial imbalances that often accompany it, allowing for targeted treatment rather than guesswork.
The Candida Confusion
If you've been researching gut health, you've likely encountered Candida as an explanation for symptoms like bloating, brain fog, fatigue, and sugar cravings. The internet is full of symptom checklists suggesting that if you answer "yes" to enough questions, Candida overgrowth is your problem.
Here's the reality: Candida can genuinely overgrow and cause problems, but it's frequently blamed for symptoms that have other causes.
Many clients come to us convinced they have Candida overgrowth—sometimes after years of anti-Candida diets and supplements—only to discover through testing that their Candida levels are normal. Their symptoms were being driven by bacterial imbalances, SIBO, or other factors entirely.
This doesn't mean Candida overgrowth isn't real. It means that assuming Candida is the problem without testing often leads to ineffective treatment and prolonged suffering.
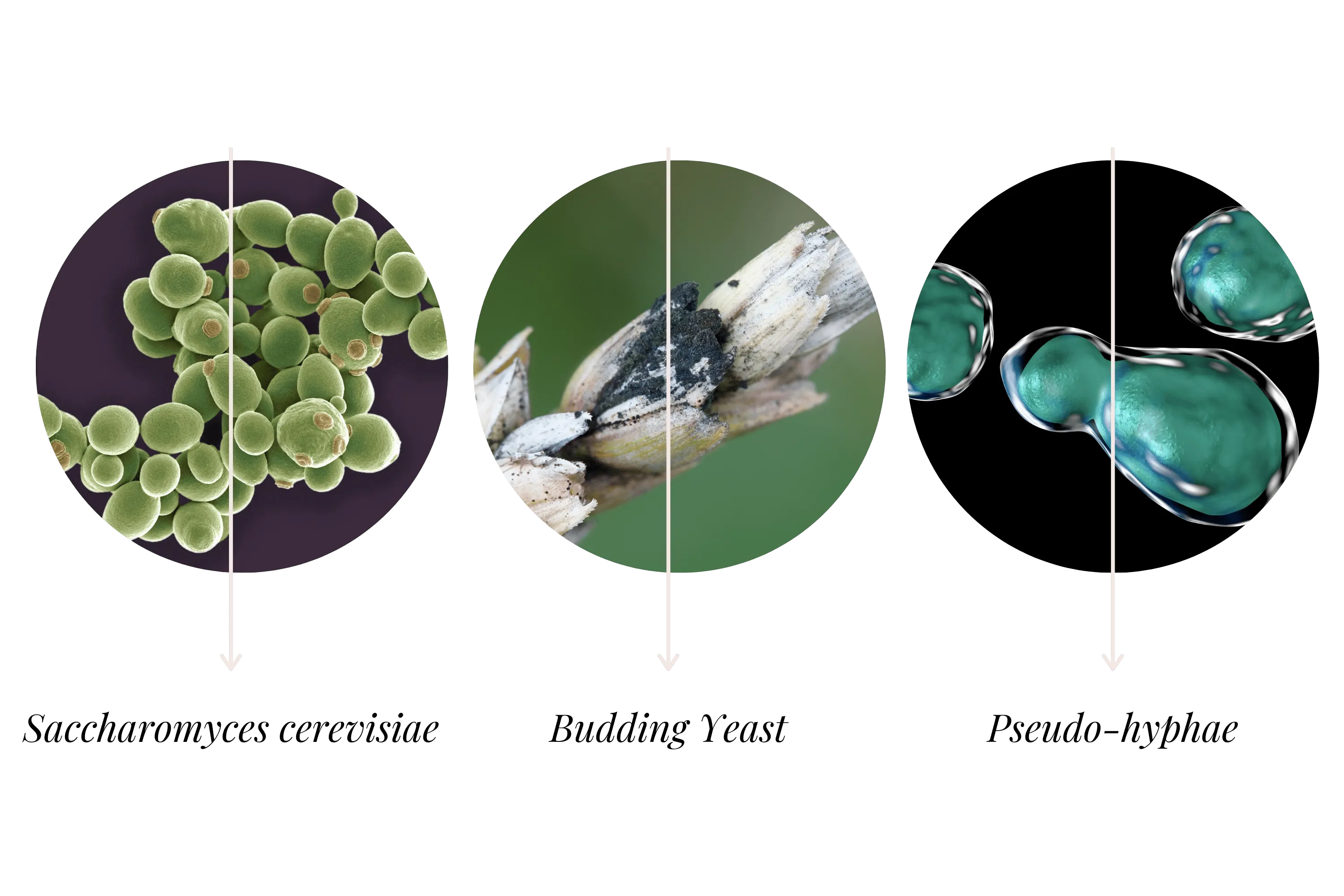
What Is Candida?
Candida is a polymorphic yeast—a type of fungus—that naturally inhabits the human body. The name derives from the Latin candidus, meaning white, describing the glossy white colonies it forms (visible as the white coating in oral thrush or vaginal discharge).
Key characteristics:
Normal inhabitant: Candida naturally lives in the gut, mouth, and vagina in most people
Sugar-dependent: Candida uses sugars as its primary energy source and is an efficient fermenter
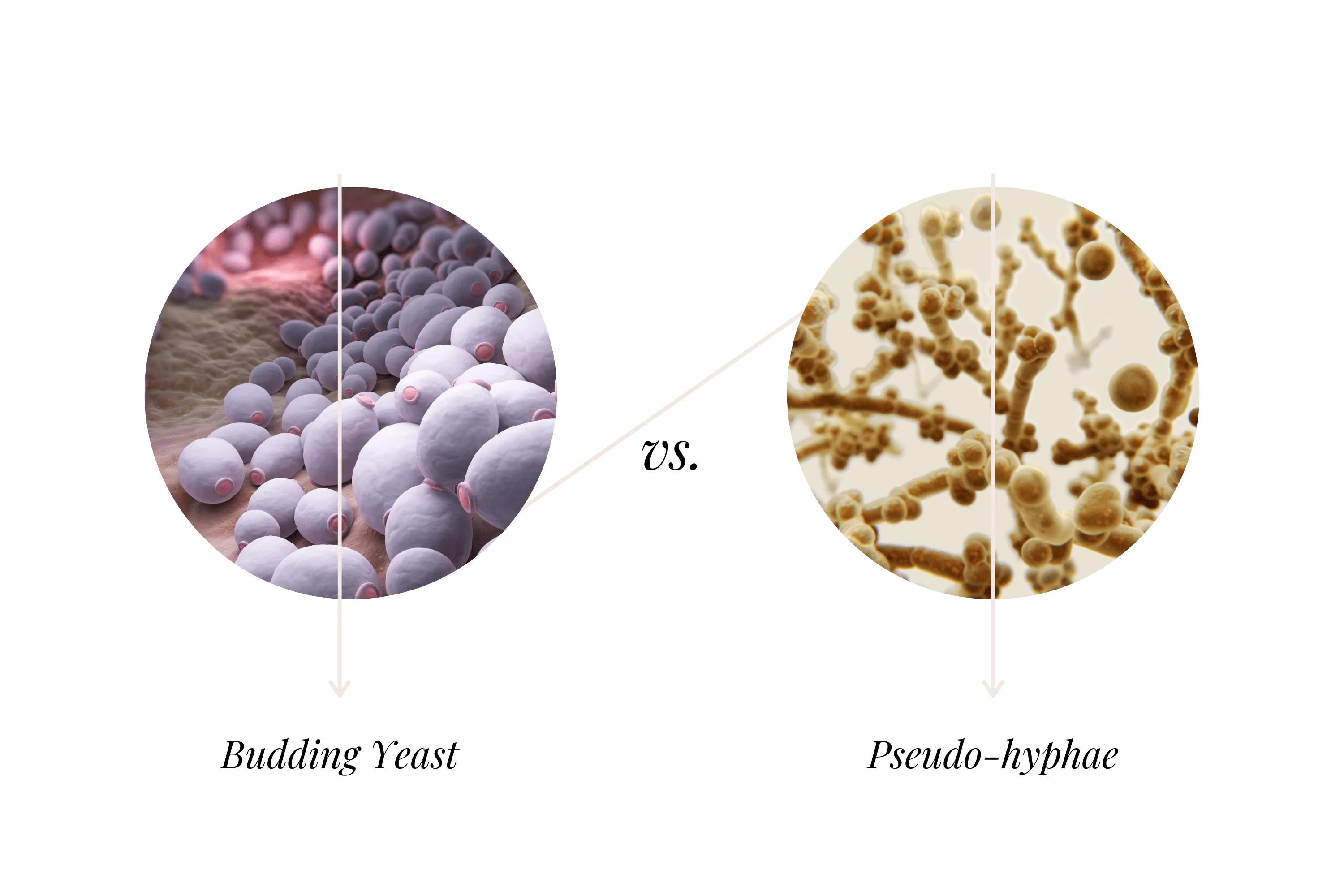
Polymorphic: It can exist in multiple forms—as rounded yeast cells or as invasive branching filaments (hyphae) that can penetrate tissues
Biofilm-forming: Candida can create protective biofilm communities with other microbes, making it difficult to eradicate
The most common species affecting humans is Candida albicans, though others like C. parapsilosis, C. krusei, and C. tropicalis can also cause overgrowth.
Under normal circumstances, beneficial bacteria—particularly Lactobacillus species—keep Candida populations in check. Problems arise when this balance is disrupted.
When Candida Becomes Problematic
In a balanced microbiome, Candida exists as a commensal—present but not causing harm. However, when conditions favour fungal growth over bacterial balance, Candida can become opportunistic.
How Candida Causes Damage
When overgrowth occurs, Candida can:
Penetrate the gut lining: Its hyphal (filament) form can directly damage gut lining cells, contribute to intestinal permeability, and trigger inflammation.
Form protective biofilms: These mucus-coated communities adhere to the gut lining and resist treatment, which is one reason Candida can be difficult to eliminate.
Produce harmful byproducts: Candida fermentation produces ethanol (alcohol), which the liver converts to acetaldehyde—the compound responsible for hangover symptoms. Chronic low-level acetaldehyde production depletes glutathione, B vitamins, and liver enzymes.
Interact with other microbes: Research shows Candida often thrives alongside Streptococcus species and Prevotella, while reduced Bacteroides and Lactobacillus populations allow Candida to flourish.
Does Candida Cause Leaky Gut?
This is where the picture becomes more nuanced.
Candida can certainly contribute to intestinal permeability. Its invasive hyphal form can create gaps in the gut lining, and the inflammation it triggers affects tight junction integrity.
However, whether Candida single-handedly causes leaky gut is a different question. In most cases, Candida overgrowth occurs alongside other factors:
Bacterial dysbiosis
SIBO (small intestinal bacterial overgrowth)
Dietary factors (high sugar, low fibre)
Antibiotic history
Chronic stress
Medication use
The clinical reality: When we test clients with suspected Candida overgrowth, we typically find multiple imbalances. Candida may be elevated, but so are certain bacterial species, and beneficial bacteria are often depleted. Addressing only the fungal component while ignoring bacterial dysbiosis rarely produces lasting results.
This is why testing matters—it reveals what's actually present rather than what symptoms suggest might be present.
🔬 VICTORIA'S EXPERT INSIGHT
"When I review test results for clients who've been treating 'Candida' for years without improvement, I often find their Candida levels are actually within normal range. What's driving their symptoms is bacterial dysbiosis—elevated Streptococcus or Klebsiella, depleted Lactobacillus and Bifidobacterium, or patterns suggesting SIBO. Conversely, I do see genuine Candida overgrowth that standard tests miss entirely because most bacterial-focused tests don't assess fungi. Metagenomic sequencing detects both, which is why it reveals what's actually happening rather than what we assume is happening based on symptoms."
— Victoria, Microbiologist
Book Your Free Evaluation Call
The Problem with Symptom-Based Diagnosis
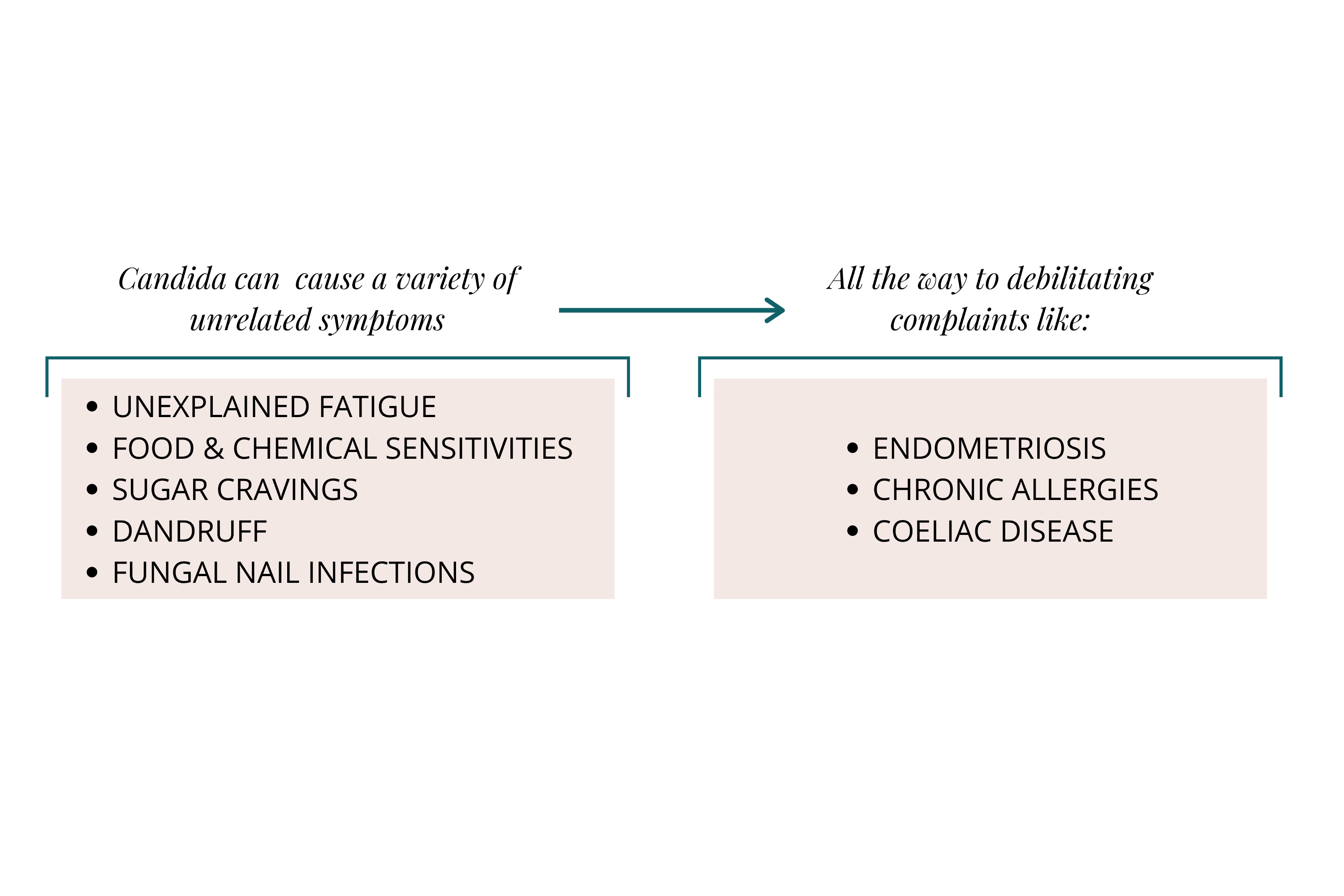
Candida overgrowth has been attributed to an extraordinarily wide range of symptoms:
Bloating, gas, constipation, diarrhoea
Fatigue and brain fog
Sugar cravings
Oral or vaginal thrush
Skin issues (acne, psoriasis, fungal infections)
Mood changes and irritability
Joint pain
Chemical sensitivities
The challenge? These same symptoms occur with bacterial dysbiosis, SIBO, food sensitivities, hormonal imbalances, and numerous other conditions.
When symptom checklists become the diagnostic tool, people often spend years on anti-Candida protocols that don't address their actual imbalances. They eliminate foods, take antifungal supplements, experience temporary improvement (often from dietary changes that would help regardless of Candida status), then relapse because the root cause was never identified.
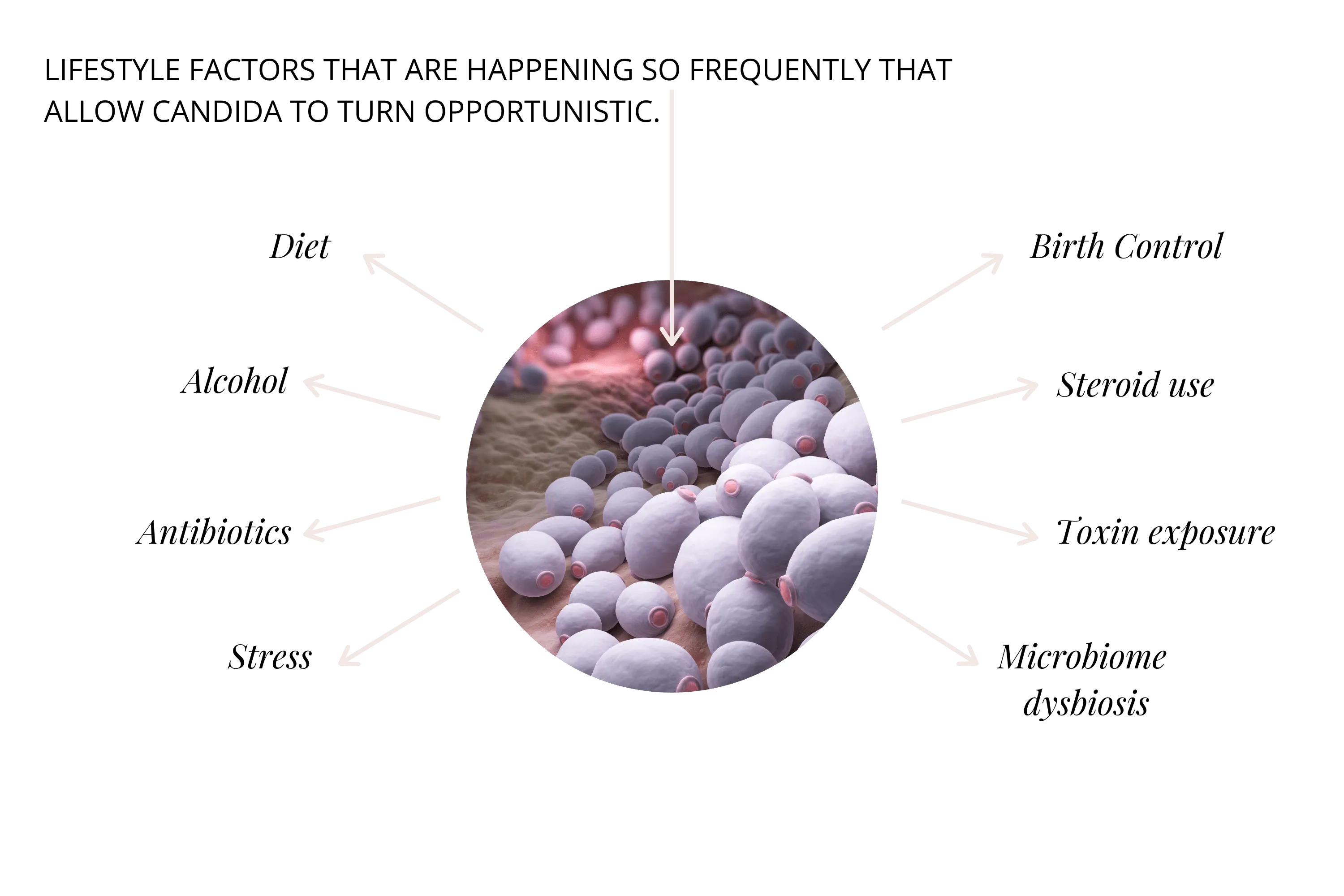
What Actually Promotes Candida Overgrowth
When genuine Candida overgrowth does occur, several factors typically contribute:
Dietary Factors
High sugar and refined carbohydrate intake (Candida's preferred fuel)
Low fibre consumption (reduces beneficial bacteria that keep Candida in check)
Alcohol consumption (fermentation products support yeast growth)
Medications
Antibiotics: Kill bacteria that normally suppress Candida
Oral contraceptives: Hormonal changes affect vaginal flora and can influence gut Candida
Corticosteroids: Inhaled corticosteroids increase Candida growth
Immunosuppressants: Reduce immune surveillance of fungal populations
Hormonal Factors
Oestrogen fluctuations affect Lactobacillus populations
Candida binds oestrogen, which promotes its growth
Xenoestrogens (environmental oestrogen mimics) may have similar effects
Microbiome Disruption
Reduced Lactobacillus and other lactic acid bacteria
General dysbiosis that allows opportunistic organisms to flourish
Compromised gut lining integrity
Other Factors
Chronic stress (creates acidic conditions favouring yeast)
High toxic burden
Weakened immune function
The Testing Difference
The fundamental issue with Candida is that symptoms alone cannot confirm or rule out overgrowth. The same symptoms arise from multiple causes, and effective treatment depends on knowing what's actually present.
What Standard Tests Miss
Most gut tests use 16S rRNA sequencing, which only assesses bacteria. They cannot detect:
Candida and other fungi
The full mycobiome (fungal community)
Whether fungal overgrowth is contributing to symptoms
This means someone could have significant Candida overgrowth that never appears on their test results.
What Comprehensive Testing Reveals
Metagenomic sequencing assesses the complete microbial picture:
Bacterial populations (beneficial and problematic)
Fungal populations including Candida species
Parasites
Viral markers
This allows for targeted treatment. If Candida is genuinely elevated, antifungal protocols make sense. If Candida is normal but bacterial dysbiosis is present, treatment should focus there instead.
A Balanced Approach to Candida
If you suspect Candida overgrowth, consider this framework:
1. Test Before Treating
Rather than assuming Candida based on symptoms, comprehensive testing confirms whether fungal overgrowth is actually present—and what else might be contributing to your symptoms.
2. Address the Full Picture
Even when Candida is elevated, it rarely exists in isolation. Effective treatment typically requires:
Reducing Candida populations
Rebuilding beneficial bacteria (especially Lactobacillus)
Addressing any bacterial dysbiosis
Supporting gut lining repair
Modifying dietary factors
3. Support Bacterial Balance
The bacteria that keep Candida in check need support:
Prebiotics feed beneficial bacteria
Probiotics—particularly Lactobacillus strains—help restore balance
Fermentable fibre supports SCFA production
Note: Some fermented foods contain yeasts and may not be appropriate during active Candida treatment. Work with a practitioner to determine what's suitable for your situation.
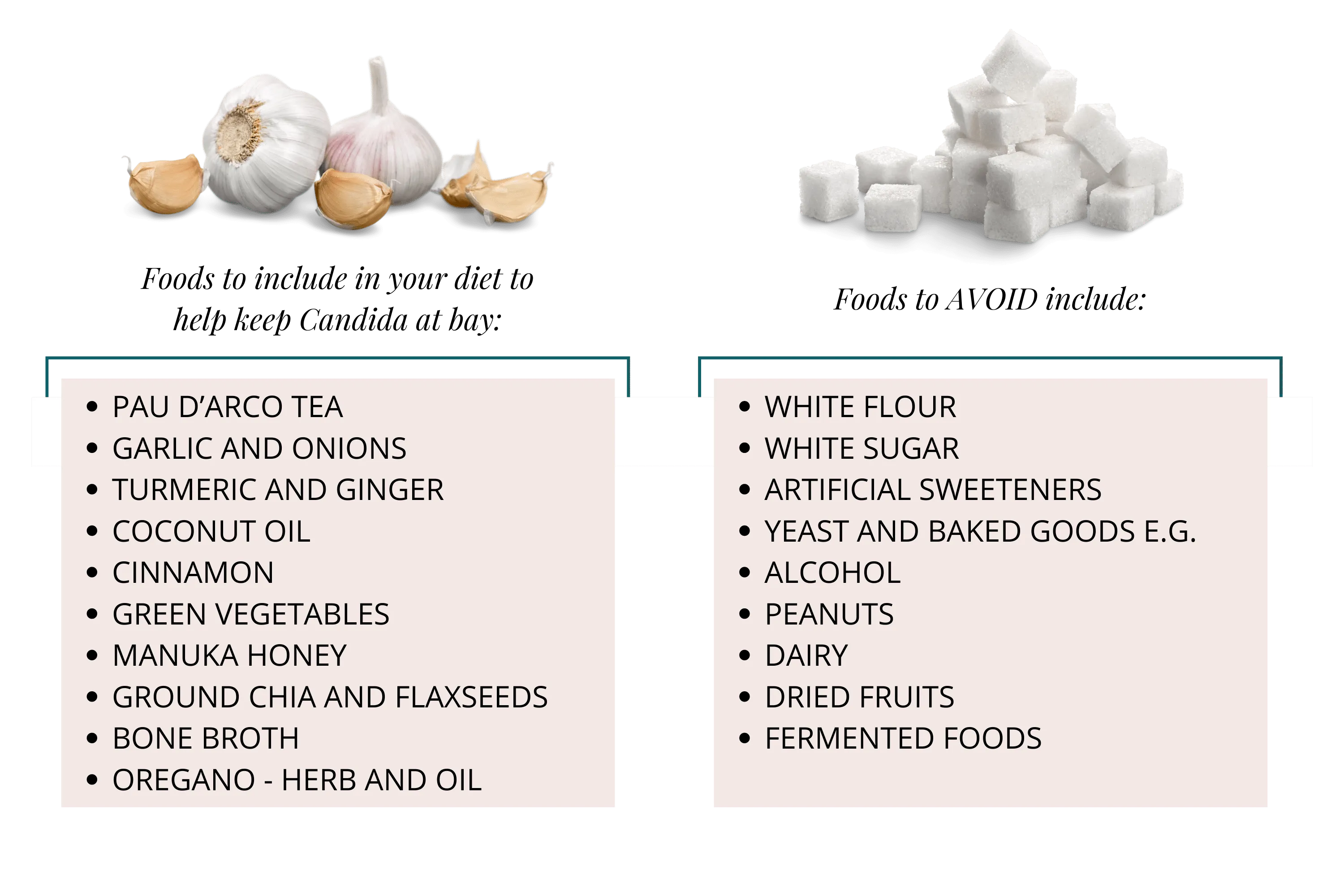
4. Reduce Candida-Promoting Factors
Minimise refined sugars and simple carbohydrates
Address alcohol consumption
Review medications with your healthcare provider
Manage stress
Reduce environmental toxin exposure
5. Expect Die-Off
When Candida populations decrease, their breakdown releases toxins that can temporarily worsen symptoms:
Fatigue
Headaches
Digestive upset
Flu-like feelings
This typically resolves within a week and indicates treatment is working. A practitioner can help manage die-off and adjust treatment pace.

Ready for Answers Instead of Assumptions?
If you've been treating suspected Candida without lasting improvement—or you're wondering whether Candida is actually contributing to your symptoms—testing provides clarity.
At Prana Thrive, we use comprehensive metagenomic testing that assesses both bacterial and fungal populations, revealing whether Candida is genuinely elevated and what other imbalances may be present. Every test is reviewed by Amanda (who has personally analysed over 2,000 individual microbiome tests) with scientific oversight from Victoria, our in-house microbiologist.
Our AIM Method™ (Analyse → Integrate → Monitor) provides:
Analyse: Comprehensive testing reveals your actual fungal and bacterial populations—confirming or ruling out Candida overgrowth and identifying other contributing factors
Integrate: A personalised protocol addressing what's actually present, not what symptoms suggest might be present
Monitor: Follow-up testing to confirm Candida reduction and bacterial rebalancing, ensuring lasting results rather than temporary improvement
Book a free 15-minute evaluation call to discuss your symptoms and find out if our testing-guided approach is right for you.
We work with a limited number of clients each month to ensure everyone receives the attention they deserve. If you're ready to know what's actually happening in your gut—rather than guessing—book your call now.
Book Your Free Evaluation Call
Related Articles:
Service Pages:

