Gut-Thyroid Connection: How Your Gut Bacteria Influence Thyroid Health
Author:
Amanda Ledwith, BHSc Naturopathy
Last Updated:
23 Jan 2026
Reading Time:
12 mins
Categories:
Gut Connections
gut-thyroid-connection
What You'll Learn
Your gut microbiome directly influences thyroid function through multiple mechanisms: nutrient absorption (iodine, selenium, zinc, iron), T4 to T3 hormone conversion, immune regulation, and inflammation control.
Research shows that autoimmune thyroid conditions like Hashimoto's and Graves' disease frequently co-occur with gut disorders, and specific bacterial imbalances—including reduced Bifidobacterium and Lactobacillus—are consistently found in thyroid disease.
Lipopolysaccharides (LPS) from certain gut bacteria can decrease thyroid hormone levels, reduce thyroid receptors, and contribute to autoimmune thyroiditis. Addressing gut health through testing and targeted interventions is often essential for supporting thyroid function.
Why Thyroid Health Matters
Constant fatigue. Difficulty regulating body temperature. A metabolism that seems stuck in the wrong gear. If these symptoms sound familiar, thyroid dysfunction may be a factor—and it's more common than many people realise.
Thyroid and autoimmune thyroid diseases are among the most prevalent medical conditions globally. Hashimoto's thyroiditis alone affects 10–12% of the population worldwide, while iodine-deficiency goitre affects an estimated 200 million people.
Your thyroid is responsible for critical metabolic functions:
Energy production and metabolism
Body temperature regulation
Immune system function
Growth and tissue repair
What's increasingly clear from research is that gut health plays a significant role in thyroid function—and addressing the gut is often essential for supporting the thyroid.
Understanding Your Thyroid
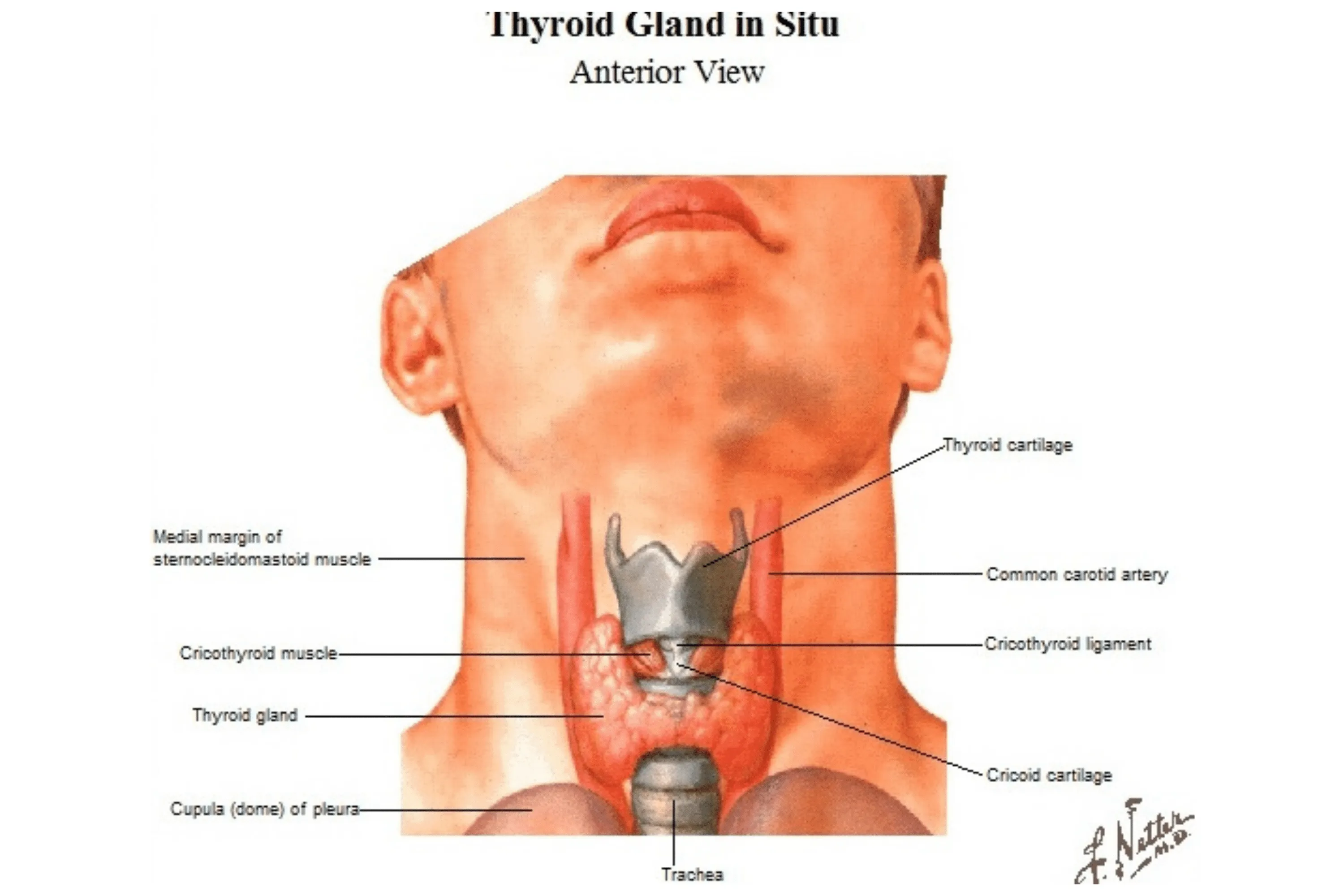
The thyroid is your largest endocrine (hormone-producing) gland, though it weighs only about 20 grams. Located just below your voice box, this butterfly-shaped gland contains follicles filled with thyroglobulin—a protein bound to thyroid hormones.
Behind each thyroid lobe sit four parathyroid glands, which release parathyroid hormone (PTH) to regulate calcium levels. PTH primarily targets bone, kidneys, and intestines—illustrating that different tissues respond to different hormones.
Thyroid Hormones Explained
Your thyroid secretes two major hormones: T3 (triiodothyronine) and T4 (thyroxine). These hormones increase metabolic rate and are essential for normal growth. Most cells in the body respond to T3 and T4.
The key difference: T4 is the inactive form that's converted to active T3 for use throughout the body. This conversion process generates free radicals through oxidation reactions—which is why antioxidant nutrients like selenium and glutathione are important for thyroid health.
A blood test can measure your free T3 and T4 levels, providing insight into thyroid function.
Supporting Hormones
Several other hormones work with T3 and T4:
TSH (thyroid-stimulating hormone): Promotes thyroid hormone synthesis. For TSH to work effectively, iodine must be available—making iodine status crucial for thyroid function.
TBG (thyroid-binding globulin): Produced by the liver, TBG binds to T3 and T4 in the bloodstream, extending their lifespan and maintaining steady hormone concentrations in cells.
TRH (thyroid-releasing hormone): Released from the hypothalamus in the brain, TRH works with TSH to regulate T3 and T4 secretion.
This complex interplay explains why thyroid problems are so prevalent—optimal function requires precise balance across multiple systems.
Why Thyroid Hormones Affect Everything
Unlike some hormones that target specific tissues, thyroid hormones affect nearly every cell in the body. However, different tissues respond in different ways.
Metabolic Effects
Increased rate of glucose, fat, and protein metabolism
Blood cholesterol level reduction
Body temperature regulation (through sodium-potassium ion exchange)
Mitochondrial activity—affecting energy and heat production
Normal metabolism and body temperature require adequate thyroid hormone levels. Low levels produce the opposite effects.
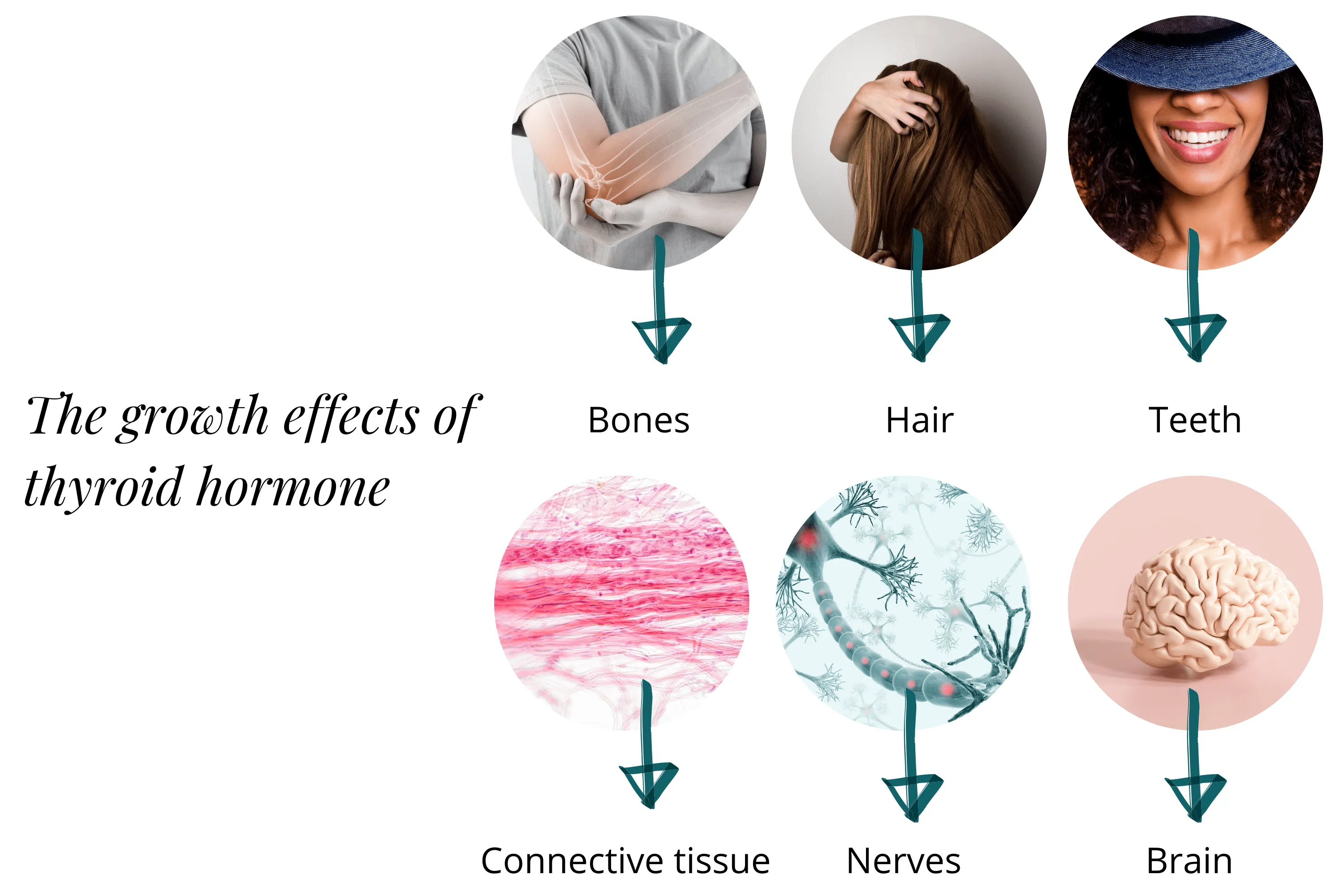
Growth Effects
Adequate thyroid hormone is essential for development and maintenance of:
Bones
Hair
Teeth
Connective tissue (including muscles)
Nervous system
Brain
Hyperthyroidism vs Hypothyroidism
Thyroid dysfunction generally moves in two directions: too much hormone (hyperthyroidism) or too little (hypothyroidism).
Hyperthyroidism Symptoms
Weight loss despite increased appetite
Rapid heartbeat, palpitations
Heat intolerance, excessive sweating
Anxiety, irritability, tremors
Difficulty sleeping
Frequent bowel movements
Enlarged thyroid (goitre)
Hypothyroidism Symptoms
Weight gain, difficulty losing weight
Fatigue, sluggishness
Cold intolerance
Depression, brain fog
Dry skin, hair loss
Constipation
Enlarged thyroid (goitre)
Both conditions can cause thyroid enlargement, though through different mechanisms.
Conditions Associated with Hyperthyroidism
Graves' disease — Autoimmune condition characterised by goitre and protruding eyes
Thyroid tumours — Including pituitary tumours (elevated TSH)
Viral thyroiditis
Thyroid storm — Sudden thyroid hormone release triggered by surgery, stress, or infection
Conditions Associated with Hypothyroidism
Iodine deficiency — Causes inadequate thyroid hormone, elevated TSH, and goitre
Goitrogenic substances — Chemicals that inhibit thyroid hormone synthesis
Thyroid gland removal
Pituitary insufficiency — Inadequate TSH secretion
Hashimoto's disease — Autoimmune condition with depressed thyroid function
The Gut-Thyroid Connection
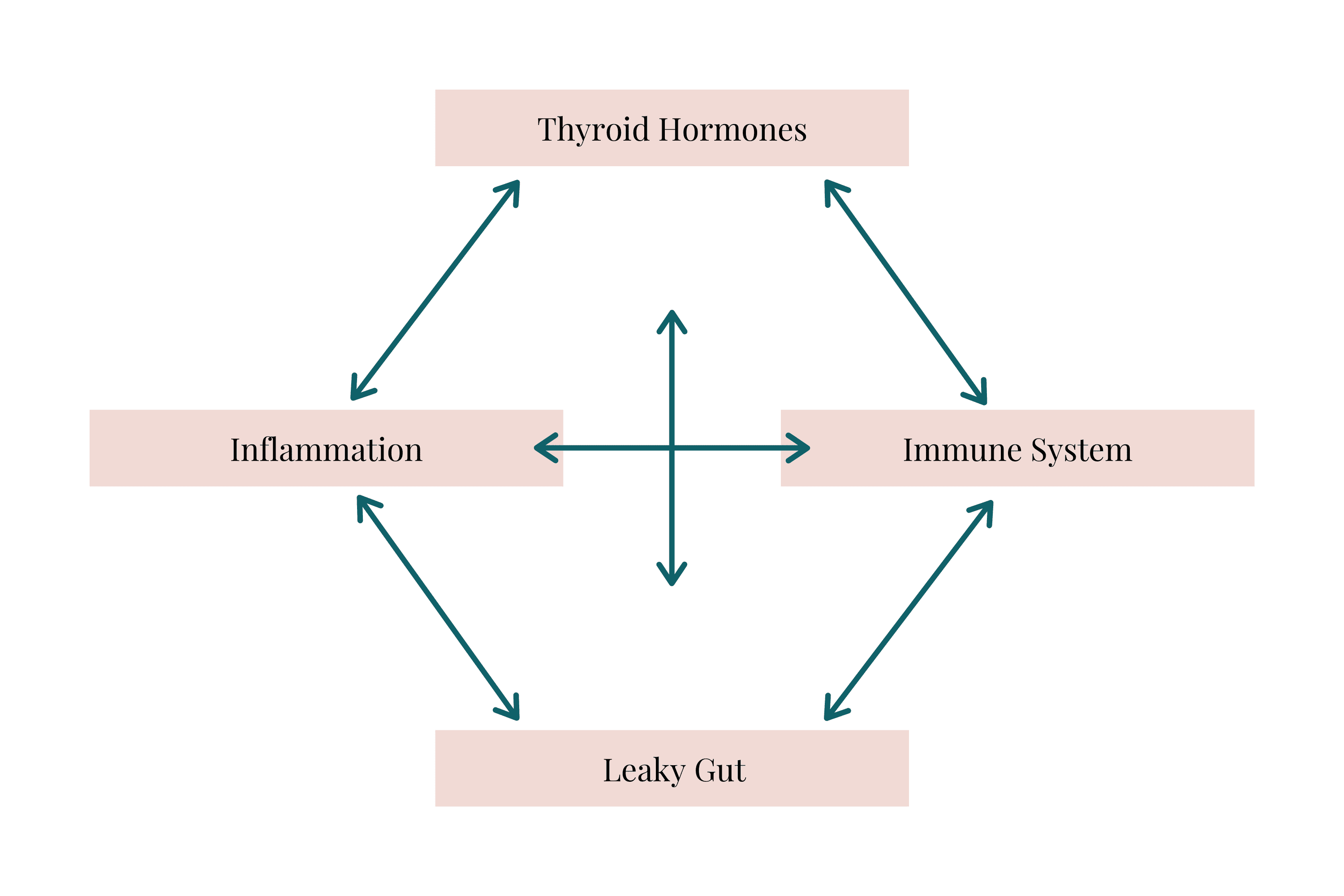
Research increasingly reveals that gut health and thyroid function are deeply interconnected.
The two most common autoimmune thyroid diseases—Hashimoto's and Graves'—frequently co-occur with coeliac disease and non-coeliac wheat sensitivity. Both conditions involve inflammation and compromised gut lining integrity.
A damaged gut lining allows antigens and reactive substances to pass into the bloodstream, triggering immune reactions and sensitivities. This connection is particularly relevant given the autoimmune component of many thyroid conditions.
How the Gut Influences the Thyroid
Gut lining integrity: Thyroid hormones directly affect tight junctions in the gut. You can read more about tight junctions and gut lining anatomy here.
Immune system development: TRH and TSH both influence the development of gut-associated lymphoid tissue (GALT)—which comprises approximately 70% of the immune system.
Microbiome balance: Gut dysbiosis has been found in many thyroid diseases, including thyroid cancer.
Nutrient availability: Gut bacteria influence the absorption and availability of thyroid-essential micronutrients:
Iodine, iron, and copper — Essential for thyroid hormone synthesis
Selenium and zinc — Required for T4 to T3 conversion
Vitamin D — Regulates immune response
These micronutrients are often deficient in people with autoimmune thyroid diseases—and gut health directly affects their absorption.
Additionally, certain gut bacteria assist in the conversion of T4 to T3, making the microbiome a direct participant in thyroid hormone activation.
Specific Bacterial Connections to Thyroid Disease
Research reveals distinct bacterial patterns in thyroid conditions.
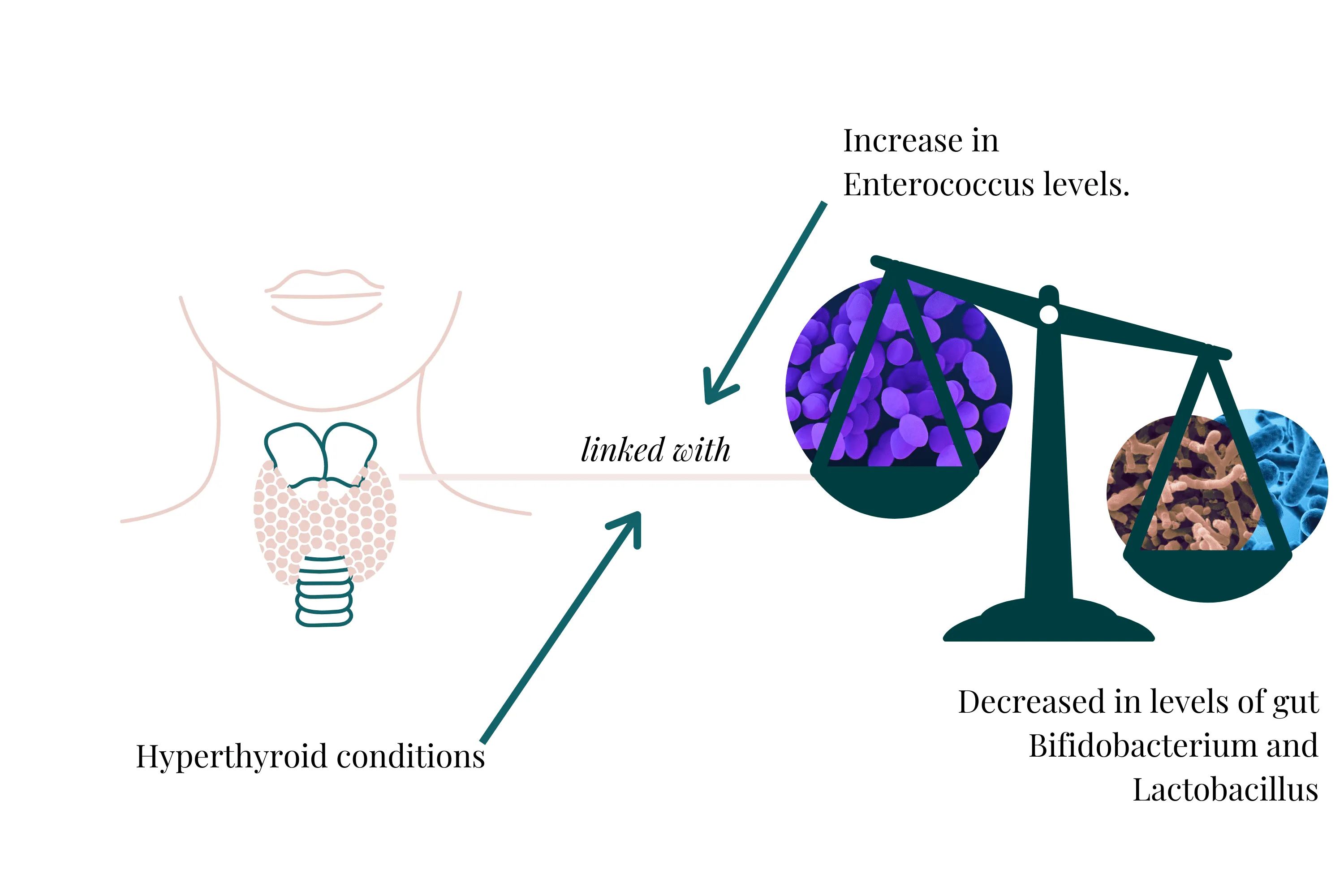
Hyperthyroidism
Studies show significant decreases in Bifidobacterium and Lactobacillus alongside increased Enterococcus levels in hyperthyroid conditions.
Bifidobacterium and Lactobacillus play crucial roles in microbiome health, producing short-chain fatty acids (SCFAs) that reduce inflammation and support gut lining cells. Their depletion compromises these protective functions.
Hypothyroidism
Research on hypothyroid gut dysbiosis shows decreased SCFA production, indicating increased inflammation. Specific bacteria like Veillonella appear elevated in hypothyroid presentations.
Notably, hypothyroid individuals also show increased blood levels of lipopolysaccharides (LPS)—a significant finding given LPS's effects on thyroid function.
🔬 VICTORIA'S EXPERT INSIGHT
"When I analyse microbiome results for clients with thyroid concerns, I specifically assess Bifidobacterium and Lactobacillus populations, markers of intestinal permeability, and indicators of LPS-producing bacteria. The pattern I frequently see in Hashimoto's clients is reduced beneficial bacteria alongside elevated opportunistic species that contribute to gut permeability—creating a cycle where bacterial toxins like LPS continuously trigger immune responses. Breaking this cycle requires addressing the specific bacterial imbalances, not just supporting thyroid hormone levels. This is why clients often see thyroid improvements when we focus on restoring gut bacterial balance."
— Victoria, Microbiologist
Book Your Free Evaluation Call
The LPS Connection
Lipopolysaccharide (LPS) is a structural component of certain bacterial cell walls. When these bacteria are abundant and the gut lining is permeable, LPS enters the bloodstream and triggers immune responses.
Research shows LPS negatively affects thyroid function in multiple ways:
Decreases thyroid hormone levels
Reduces thyroid hormone receptors
Contributes to autoimmune thyroiditis and goitre development
Reduces thyroid-stimulating hormone (TSH)
Increases inactive T3 (reverse T3)
This explains why addressing gut permeability and bacterial balance is often essential for supporting thyroid health—even when thyroid hormone supplementation is already in place.
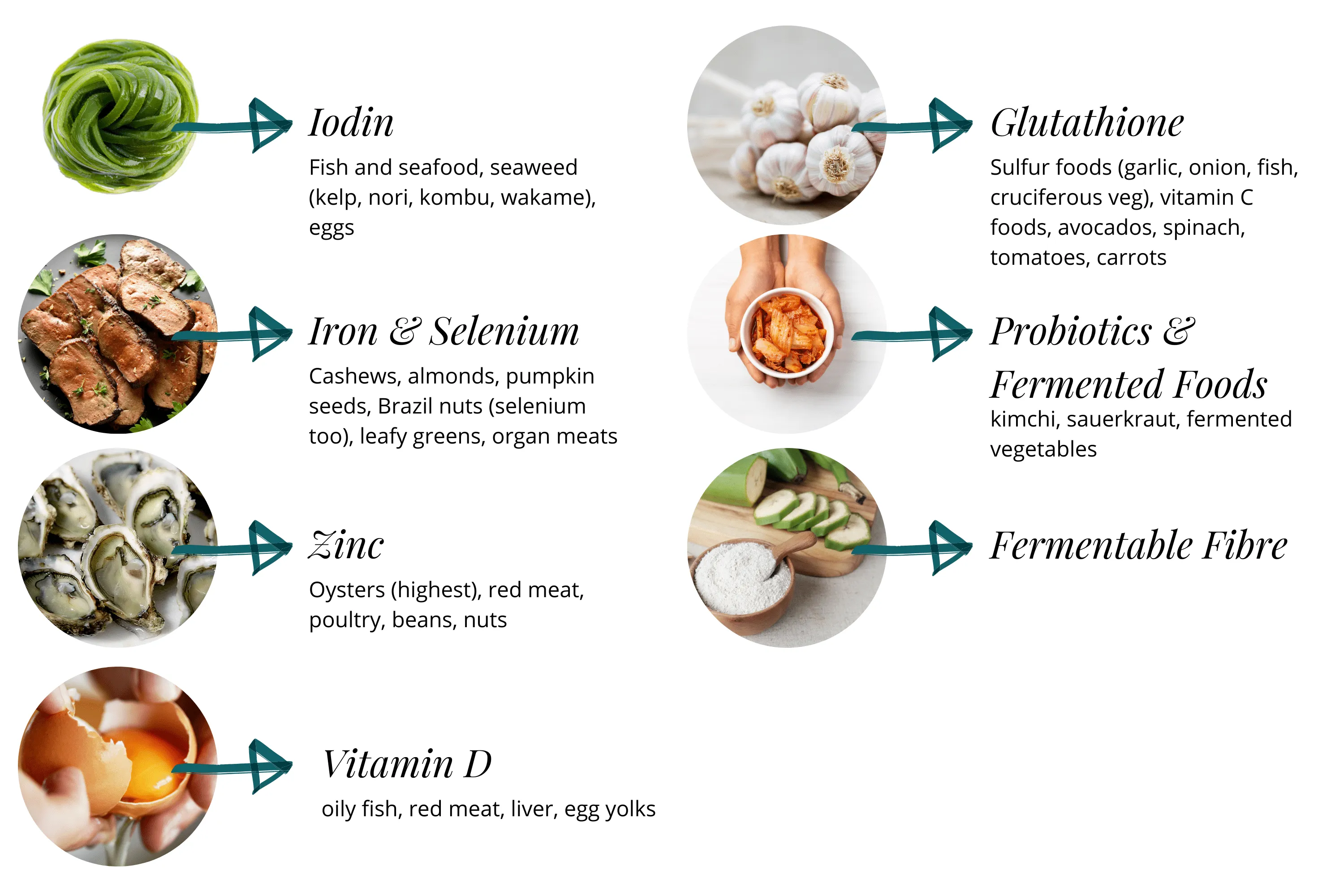
Nutrients Essential for Thyroid Health
Several nutrients are critical for thyroid function, and gut health directly affects their absorption.
Iodine
Essential for thyroid hormone synthesis. Without adequate iodine, the thyroid cannot produce T3 and T4.
Food sources: Fish and seafood, seaweed (kelp, nori, kombu, wakame), eggs
Iron
Required for iodine absorption and thyroid hormone synthesis. Iron deficiency is common in hypothyroidism.
Food sources: Organ meats, leafy greens, legumes
Selenium
A potent antioxidant critical for neutralising free radicals generated during thyroid hormone synthesis. Also required for T4 to T3 conversion.
Food sources: Brazil nuts (highest), cashews, pumpkin seeds
Zinc
Essential for T4 to T3 conversion. Zinc deficiency commonly presents with thyroid conditions. Zinc is primarily absorbed in the gut, making gut health critical for zinc status.
Food sources: Oysters (highest), red meat, poultry, beans, nuts
Vitamin D
Regulates immune function and protects against autoimmunity. Low levels are seen in hypothyroidism. Vitamin D2 comes from food; D3 is produced in the skin from sunlight exposure.
Food sources: Oily fish, red meat, liver, egg yolks
Note: Adequate sun exposure supports vitamin D synthesis.
Glutathione
A master antioxidant that plays an important role in T4 to T3 conversion, helps neutralise free radicals, and maintains thyroid tissue health. Learn more about glutathione and how to support it.
Food sources: Sulphur-rich foods (garlic, onion, cruciferous vegetables), vitamin C foods, avocados, spinach
Note: NSAIDs like paracetamol deplete liver glutathione stores.
Supporting Thyroid Health Through Your Gut
Beyond nutrient support, several strategies target the gut-thyroid connection directly.
Probiotics and Fermented Foods
Fermented foods provide beneficial Lactobacillus and Bifidobacteria alongside the substrates they thrive on. Lactobacillus reuteri has been specifically connected with better thyroid health.
Food sources: Kimchi, sauerkraut, fermented vegetables, miso, kefir
Important: If purchasing fermented foods, ensure they're unpasteurised—heat treatment destroys beneficial bacteria.
For more on beneficial bacteria, see our comprehensive probiotics guide.
Fermentable Fibre and Prebiotics
Fibre and resistant starch that reach the colon intact are fermented by bacteria, producing protective short-chain fatty acids. Butyrate in particular provides energy for gut cells and supports gut lining integrity.
Food sources: See 27 High-Fibre Low-Carb Foods and our comprehensive prebiotics guide
Tip: Add fibre-rich toppings to salads—chia seeds, flaxseeds, and pumpkin seeds are excellent options.
Reducing Inflammation Triggers
Common inflammation triggers can exacerbate both gut and thyroid issues, particularly in those with autoimmune thyroid conditions. Gluten, dairy, processed foods, and refined grains may need elimination or reduction.
Working with a qualified practitioner can help identify individual triggers through systematic elimination and reintroduction.
Balancing Your Microbiome
One of the most powerful interventions for thyroid health is addressing specific microbiome imbalances. This requires knowing which bacteria are elevated, which are depleted, and how they're affecting gut permeability and inflammation.
Gut microbiome testing reveals these patterns, allowing for targeted rather than generic interventions.
Ready to Address the Gut-Thyroid Connection?
Supporting thyroid health often requires looking beyond the thyroid itself. The gut's influence on nutrient absorption, hormone conversion, immune regulation, and inflammation means that gut health is frequently a foundational piece of the thyroid puzzle.
At Prana Thrive, we use comprehensive metagenomic testing to identify specific bacterial imbalances relevant to thyroid health—including Bifidobacterium and Lactobacillus levels, markers of gut permeability, and LPS-producing bacteria. Every test is reviewed by Amanda (who has personally analysed over 2,000 individual microbiome tests) with scientific oversight from Victoria, our in-house microbiologist.
Our AIM Method™ (Analyse → Integrate → Monitor) provides:
Analyse: Comprehensive testing reveals your unique bacterial profile, including species linked to thyroid function, nutrient absorption capacity, and inflammation markers
Integrate: A personalised protocol addressing your specific gut imbalances while supporting thyroid-essential nutrients and reducing inflammation triggers
Monitor: Follow-up testing and consultations to track bacterial changes and correlate with thyroid function improvements
Book a free 15-minute evaluation call to discuss your symptoms and find out if our testing-guided approach is right for you.
We work with a limited number of clients each month to ensure everyone receives the attention they deserve. If you're ready to address the gut factors affecting your thyroid—book your call now.
Book Your Free Evaluation Call
Related Articles:
Service Pages:

