What Is The Estrobolome?: Demystifying The Estrogen Gut-Hormone Connection
Author:
Amanda Ledwith, BHSc Naturopathy
Last Updated:
19 Jan 2026
Reading Time:
17 mins
Categories:
Gut Connections
estrogen-gut-connection
What You'll Learn
The estrobolome is a specialised collection of gut bacteria that regulate estrogen levels by metabolising and recycling estrogen in your intestines.
How it works:
Estrogen circulates through your body, then reaches the liver where it's deactivated for elimination
In the gut, certain bacteria (like Faecalibacterium prausnitzii) produce β-glucuronidase enzyme
This enzyme reactivates estrogen, allowing it to recirculate instead of being eliminated
When β-glucuronidase-producing bacteria are elevated, estrogen levels stay high
Estrogen imbalance symptoms:
High estrogen: Heavy/painful periods, PMS, hormonal acne, bloating, mood swings, weight struggles, headaches
Low estrogen: Sleep issues, dry mucosa, low libido, bone density loss, perimenopausal symptoms
Conditions linked to estrobolome dysbiosis:
Endometriosis - elevated β-glucuronidase, higher estrogen recycling, IBS-type symptoms in 90% of sufferers
PCOS - low diversity, dysbiosis contributing to insulin resistance and testosterone elevation
PMS - gut bacteria driving bloating, menstrual migraines, mood changes, cyclic acne
Why testing matters: Comprehensive microbiome testing reveals β-glucuronidase levels (gmGUS marker), which bacteria are elevated, and whether your gut is recycling too much estrogen. This guides targeted protocols to reduce estrogen-recycling bacteria and restore hormone balance.
Have you ever considered that your period (and how you feel during it) is connected to the bacteria in your gut (not just blood estrogen levels)?
So many of us struggle with hormone imbalances, whether it comes as PMS, hormonal acne, painful, heavy periods or even waking at 2am. Most of the time we just put it down to crazy hormones and stress, but not many of us make the gut-hormone connection.
Why?
Because the connection between estrogen, our primary female sex hormone, and the direct influence from our gut bacteria is only a relatively recent finding.
Research has spotlighted a complex interplay between estrogen and the gut microbiome. It has earned a new title, the estrobolome.
So, what does your period say about your gut?
A Closer Look at Estrogen

When we talk about estrogen, we are actually referring to three major hormones – estrone (E1), estradiol (E2), and estriol (E3).
Estrone (E1): Estrone is made in the ovaries prior to menopause, but can also be made in the adrenal glands and fat tissue. After menopause total estrogen levels reduce but we still produce E1.
Estradiol (E2): Estradiol is the most abundant form of estrogen we produce until menopause. It plays a significant role in breast development, female fat distribution, reproductive tissue health, bone growth, heart health, memory and cognition. Estradiol is also the form of estrogen connected with endometriosis, fibroids, breast and endometrial cancers and menstrual cycle symptoms.
Estriol (E3): Estriol is produced by the placenta in pregnancy and is the least potent form of estrogen.
Our estrogen levels fluctuate daily, monthly and over our life cycles, this is normal. What isn't normal is a pattern of imbalance. There are a couple of ways this presents:
High estrogen levels: Shows up as irregular, heavy or painful periods, mood swings, weight struggles, headaches, acne, bloating, digestive symptoms – these are all symptoms of excess estrogen. Conditions like endometriosis, fibroids and reproductive cancers are linked with estrogen levels remaining high for too long.
Low estrogen levels: Sleep issues, mood, dry mucosa, urinary tract irritation, low libido, bone density loss, perimenopausal symptoms are connected with low estrogen levels.
And this is where the estrobolome comes in – it's like a specialised department within the microbiome that regulates your estrogen levels. The bacteria involved have genes that help (sometimes too much) you metabolise estrogen.
Estrogen & The Gut Microbiome
Estrogen circulates through our bodies everyday performing its many functions like stabilising mood, keeping our cognition sharp, our hair shiny, periods regular and our bones strong.
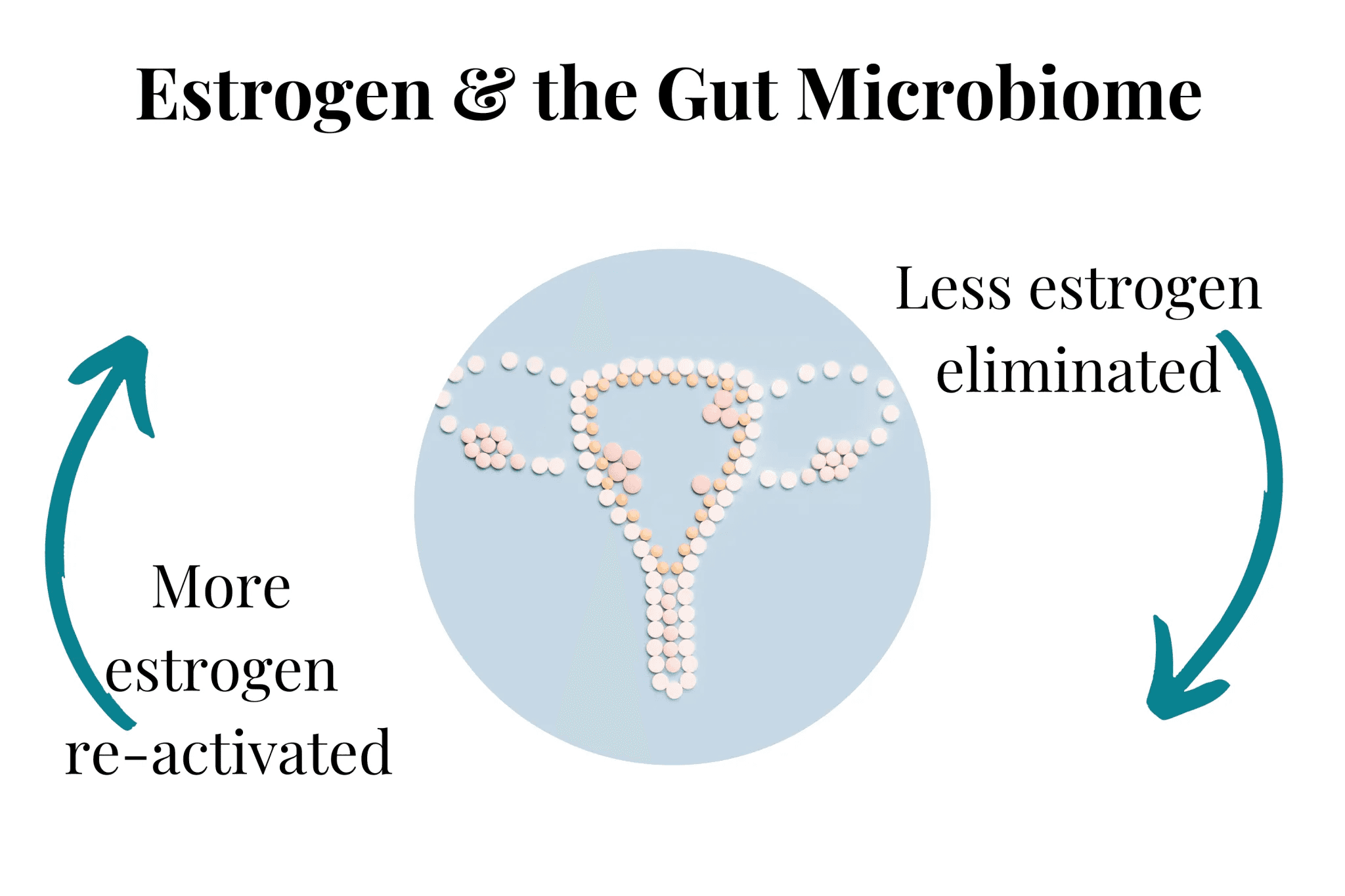
Eventually estrogen winds up in our liver where it's broken down into estrogen metabolites and deactivated for elimination or reabsorption, through our intestines.
Once in the gut the deactivated estrogen is either eliminated or reabsorbed – our gut bacteria orchestrate this balance.
To understand how estrogens interact with gut bacteria I'm going to briefly backtrack a little and talk about liver science (not too much) for some background.
How estrogens are converted (and excreted) …
As we mentioned, our liver converts estrogen into its active metabolites. It is also where estrogen deactivation occurs too, during a process called phase II liver metabolism or detoxification.
This is where the gut bacteria come in.
During phase II liver detox, hormones, chemicals, drugs and other compounds are deactivated by the attachment of various side chain molecules including glucuronic acids.
So, active hormone + glucuronic acid = deactivated hormone
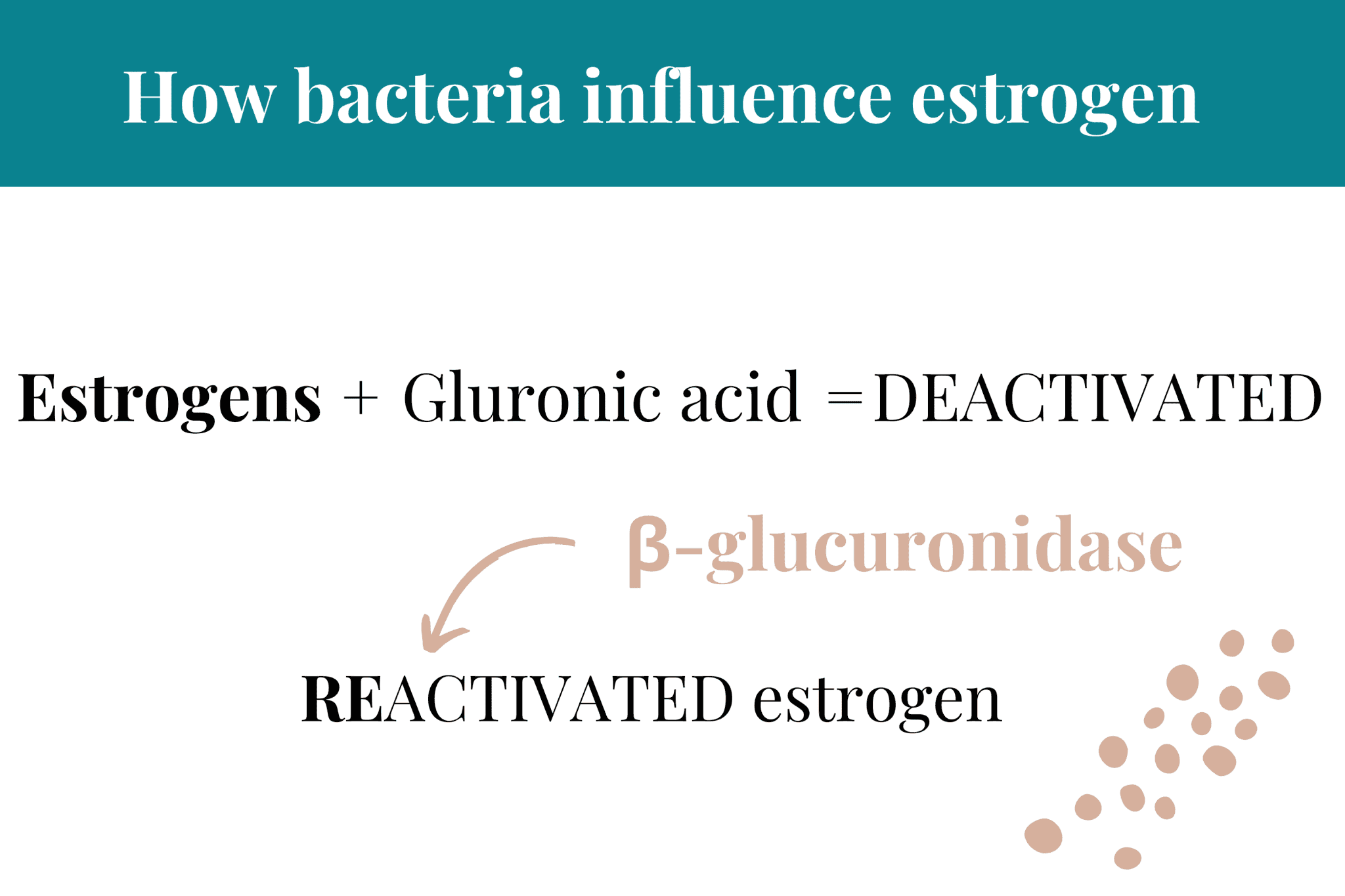
These inactivated forms are then ready for excretion along with our bile.
When they reach the gut, a number of bacteria 'see' the attached glucuronic acid side chain as a food source. But to get at it, they need to remove it from the hormone, drug or chemical it's attached to.
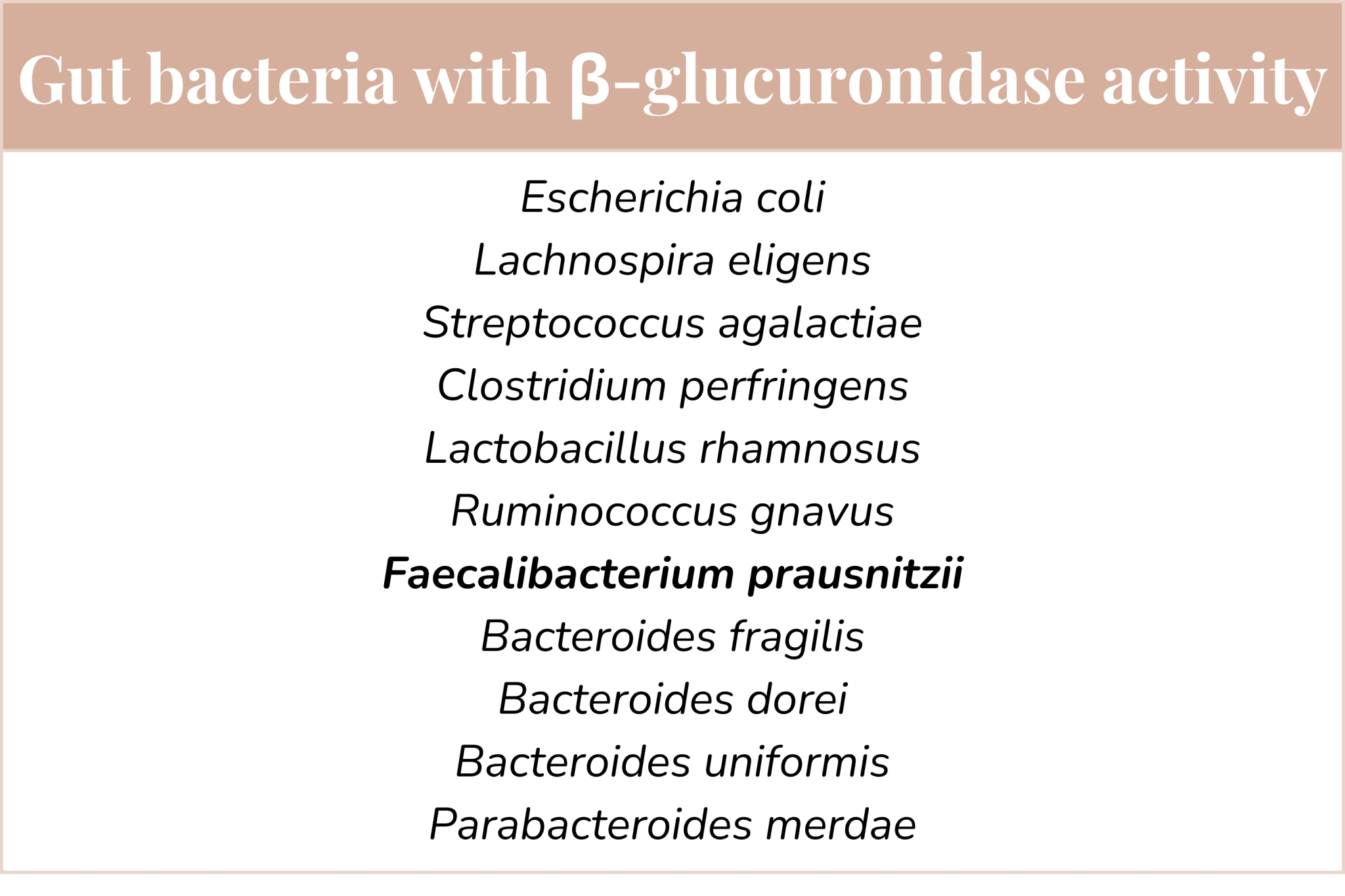
Bacteria such as Faecalibacterium prausnitzii do this.
This then leaves that meant-to-be-excreted molecule free to circulate all over again – and it is then reabsorbed.
The re-activation, recirculation and reabsorption process is particularly important in estrogen dominant conditions, like endometriosis, breast cancer etc.
Research has shown that women with these conditions, reveals an over abundance of β-glucuronidase producing species on gut microbiome test.
Knowing which microbiome species you have an abundance of, if you have an estrogen imbalance condition is a great way to support hormone balance.
🔬 VICTORIA'S EXPERT INSIGHT
"When I review microbiome test results for clients with hormone imbalances—PMS, endometriosis, PCOS, perimenopausal symptoms—I'm looking specifically at the estrobolome markers that most practitioners overlook.
What I assess in hormone-related cases:
1. β-glucuronidase (gmGUS) levels This enzyme is the key driver of estrogen recycling. When I see elevated gmGUS on test results, I know the client's gut is reactivating estrogen that should be eliminated. This explains why estrogen levels stay high despite the liver doing its job. Bacteria like Faecalibacterium prausnitzii, certain Bacteroides species, and Escherichia coli all produce this enzyme—so I look at which specific species are elevated.
2. Diversity and dysbiosis patterns In PCOS clients especially, I consistently see low diversity (200–400 range vs healthy 600+) alongside specific dysbiosis patterns. The dysbiosis contributes to insulin resistance—which then drives testosterone elevation and the classic PCOS symptoms (hair changes, acne, weight concerns). It's not just about estrogen; the whole hormonal cascade is affected by gut bacterial balance.
3. Inflammatory markers (LPS) Elevated LPS (lipopolysaccharide) from gram-negative bacteria like Proteobacteria drives systemic inflammation—which worsens both endometriosis and PCOS. When I see elevated LPS alongside elevated gmGUS, I know we need to address both the estrogen recycling AND the inflammatory bacteria driving the condition.
4. Gut barrier integrity Leaky gut is consistently present in hormone imbalance conditions. When the gut barrier is compromised, inflammatory molecules and bacterial metabolites cross into the bloodstream, triggering immune responses that worsen hormonal symptoms.
The critical insight: Hormone imbalances aren't just about blood estrogen levels—they're often driven by gut bacteria that recycle estrogen, produce inflammatory compounds, and compromise gut barrier integrity. Testing reveals these patterns, and targeted protocols can reduce β-glucuronidase-producing bacteria, lower inflammation, and restore hormone balance."
— Victoria, Microbiologist
Book Your Free Evaluation Call
How to Support Healthy Estrogen and the Microbiome
Certain plant-based foods can help us make estrogen. Leafy greens, legumes and seeds like flax contain phytoestrogens, which are structurally and functionally similar to our own estrogens.
Now you might be thinking, but isn't too much estrogen a problem … strictly yes. BUT.
Phytoestrogens can be protective to our hormonal health by blocking estrogen receptors when the levels are already too high and when estrogen is low they help keep levels supported.
We definitely also want to avoid xenoestrogens – these are estrogen mimicking chemicals found in plastics, beauty products, cleaning chemicals, mycotoxins and many other chemical or petrochemical products.
These are toxic and wreak havoc to our hormonal health.
When our gut microbiome and plant sources of phytoestrogens are in balance, everything runs smoothly with optimal levels of estrogen. It's a win-win.
Balanced estrogen supports balanced microbiome.
If things get out of balance, either from xenoestrogens, imbalanced estrobolome bacteria (or both) this is where both digestive symptoms (often leaky gut) and hormonal symptoms start to show.
It's a constant interplay between healthy microbiome and balanced estrogen – they each rely on the other.
Dysbiosis from diet, low diversity events (like from antibiotics) or overgrowth (either bacterial or fungal like Candida) can actually cause an estrogen imbalance.
And the converse is also true, estrogen levels shape the microbiome too.
Common Estrogen Imbalance Conditions
PMS: Imbalanced estrogens cause bloating, menstrual migraines, heavy periods and associated pain. Cyclic acne and the dreaded PMS mood changes are all closely connected to your gut bacteria.
Endometriosis: Women with endo have been shown to have higher rates of dysbiosis and bacterial overgrowth within the estrobolome. This leads to higher estrogen levels, which further stimulates endometrial growth. In addition to debilitating period pain and heavy bleeding, IBS symptoms are also more common alongside endometriosis, as are autoimmune symptoms.
PCOS: Low diversity with dysbiosis has been found with PCOS. The dysbiosis is thought to contribute to insulin resistance and increased testosterone production seen in PCOS. These changes drive the common symptoms of hair changes, acne and weight concerns.
How to Restore a Healthy Gut-Hormone Connection

Balancing your microbiome – along with your estrobolome – is key to hormonal health but also offers all the general wellbeing benefits of improved gut health too.
So unsurprisingly, the same fundamental things you can do for gut health everyday can make a big difference for hormone balance too. We talk in more detail about these in our online program Gut Heal & Nourish, and with our Gut Microbiome Testing clients too.
Here is a brief overview (you can read more in How To Improve Gut Health Naturally: The Ultimate Guide):
1. Remove triggers of bacterial overgrowth.
High sugar diets feed bacteria that promote inflammation and bacterial overgrowth and dysbiosis – we recommend limiting/removing sugar.
Limiting alcohol as it both raises estrogen levels but also supports non-beneficial bacterial growth.
Remove processed foods, as ultra processed foods are devoid of nutrients, minerals and fibre needed to feed beneficial bacteria but also feed the troublemakers.
Avoid environmental pollutants where possible. Pesticides, herbicides and many other environmental chemicals (including those in "treated" water) both disrupt the microbiome but also our hormones and endocrine function generally.
2. Choose microbiome feeding foods.
If you don't have significant gut health issues, adding a variety of plant foods into your diet ensures nutrient dense, phytochemical-rich (good ones), fibre, polyphenols and resistant starches are delivered to your waiting microbiome.
Increasing your cruciferous vegetables, (of course unless you've specifically been advised not to) like cauliflower, broccoli, cabbage etc. also increasing your phytoestrogens intake. They also support detoxification.
Lignan rich foods help the phytoestrogen binding site competition we mentioned above. These foods include lentils, chickpeas, whole soy products (like edamame and tofu) and flax seeds.
3. Reseed your microbiome.
Prebiotic and probiotics foods can gently balance your microbiome.
Our practitioners use a variety of supplements with pre- and pro-biotic ingredients, all selected based on gut microbiome testing.
But in general, prebiotic fibres include inulin, partially-hydrolysed guar gum, FOS (fructo-oligosaccharides, made infamous by the FODMAPs protocols) etc.
4. Follow a gut health supporting lifestyle.
Getting outside in contact with nature is an often overlooked way to boost the microbiome, and decrease stress. Stress is a known microbiome villain.
Gardening and especially organic food gardening is another way to connect with your food and your natural environment.
Shop at a local Farmers Market for super fresh and often less commercially farmed produce.
Exercise daily.
Connect with family and friends – we pass around more microbes than we do smiles sometimes.

