The Gut-Brain Connection
How Your Microbiome Affects Your Mood
Author:
Amanda Ledwith, BHSc Naturopathy
Last Updated:
16 Dec 2025
Reading Time:
XX min
Categories:
Gut Connections
gut-brain-connection
What You'll Learn
The gut-brain axis is a powerful two-way communication system between your digestive system and your central nervous system. Your gut microbiome directly influences brain function, mood, anxiety, depression, and cognitive health.
How the gut-brain connection works:
Vagus nerve — Primary communication highway carrying signals between gut and brain
Neurotransmitter production — Gut bacteria produce 90% of your serotonin, plus GABA, dopamine, acetylcholine, and melatonin
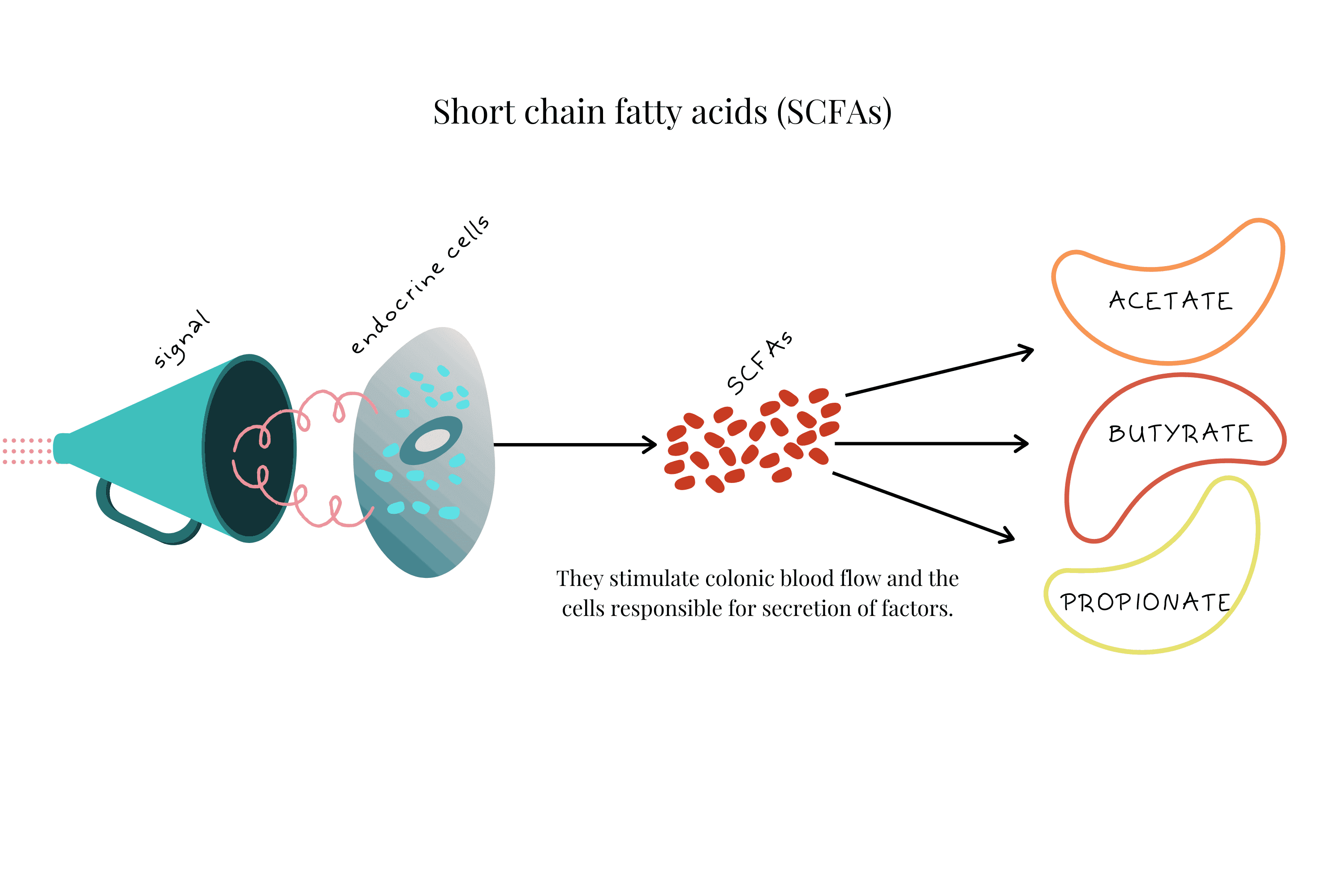
Short-chain fatty acids (SCFAs) — Bacterial metabolites like butyrate reduce neuroinflammation and support brain health
Immune signalling — Gut bacteria regulate inflammatory cytokines that affect mood and cognition
Conditions linked to gut-brain dysfunction:
Depression and anxiety
IBS (irritable bowel syndrome)
Autism spectrum disorder (ASD)
Brain fog and cognitive decline
Multiple sclerosis and neurodegenerative diseases
But here's what most people don't realise: You can eat fermented foods, take probiotics, and reduce stress—but if you don't know which bacterial species are depleted or which inflammatory bacteria are elevated, you're guessing. Testing reveals whether you're missing Faecalibacterium prausnitzii (butyrate producer linked to reduced anxiety), GABA-producing Bifidobacterium, or serotonin-supporting species.
Introduction
It's not all in your head. Medication and therapy aren't the only solutions to mental health conditions. Recent gut-brain research has found that mental health is not only a "mental" issue—it's also determined by your gut and microbiome.
The connection is undeniable. Countless scientific papers are being published daily, often pointing to the success of natural diet and lifestyle solutions. A welcome prospect for those struggling with mental illness.
People all over the world are healing.
We'll discuss some of those healing strategies in detail, with a focus on diet, lifestyle, and finding the right support.

To be clear: positive thinking, therapy, counselling, and relaxation tools all have their place and can be an important part of the healing journey.
However, science is demonstrating that part of the long-term solution lies in the simplicity of natural healing—healing your gut, supporting your liver, and building your microbiome for better brain health.
Brain fog, anxiety, depression, and other (now common) mental health conditions can improve. By focusing on your gut health, you can support your healing journey to brain wellbeing.
Here we'll discuss:
How your gut-brain connection governs your brain health
Why looking after your microbiome drives your mental wellbeing
Mental conditions associated with gut health
Ways to improve and support your gut health for mental health
When diet and lifestyle aren't enough—and why testing matters
Your Incredible Gut-Brain Connection
The connection between your digestive system and your brain has many names:
Microbiota-gut-brain axis
Brain-gut-microbiome axis
Microbiome-gut-brain connection
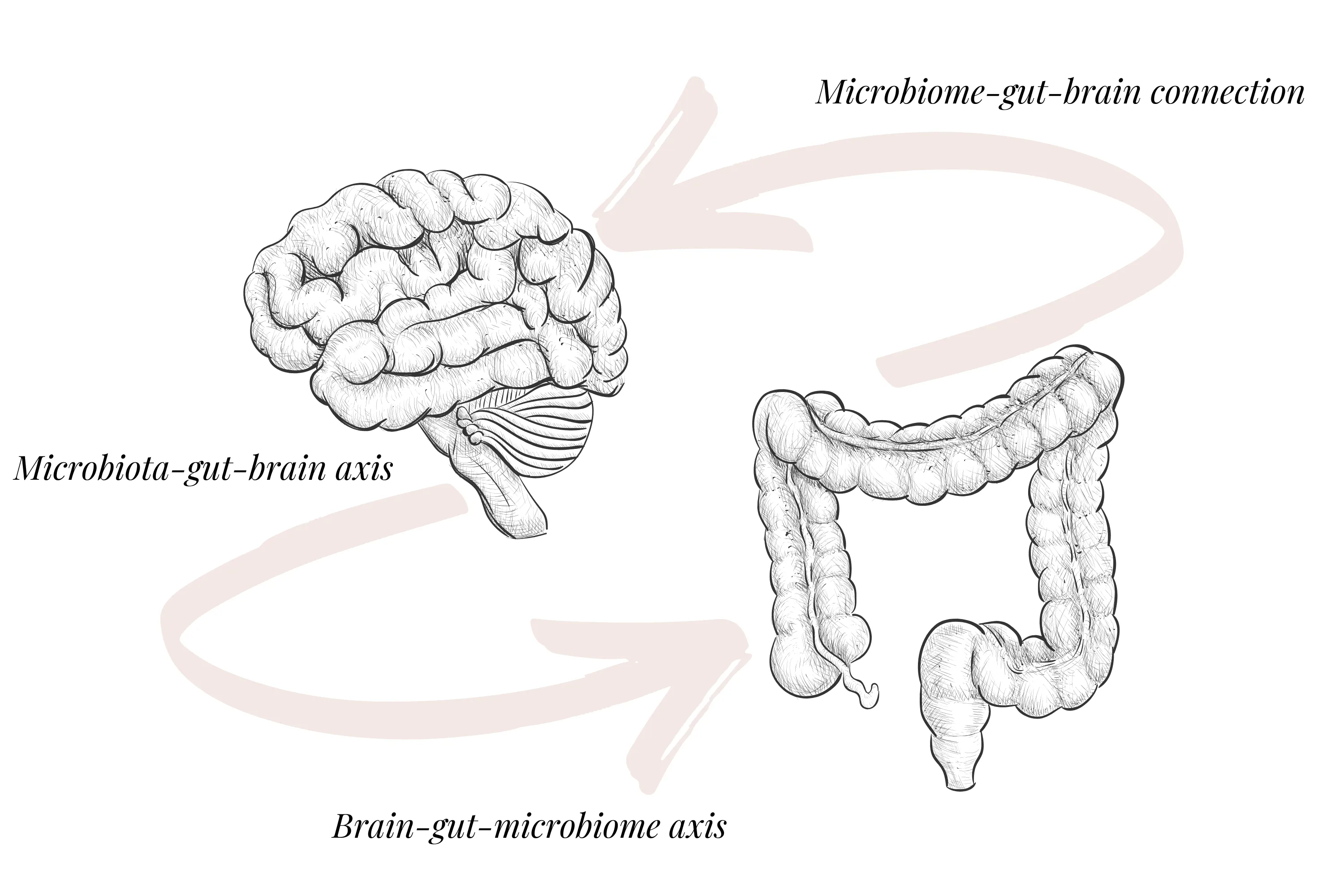
Here we'll call it the gut-brain axis or GBA for short.
Each of these names describes the gut-brain connection between your gut, its microbiome, and your central nervous system (CNS—your brain).
This two-way communication highway, working every moment, maintains balance and health for you.
Feeling low, unable to think clearly, or experiencing other minor neurological symptoms are hints—your body's clues that you have an imbalance somewhere in your system.
You may already know your gut acts as a second brain, being home to hundreds of millions of neurons. Unconsciously, we've long assumed a connection between our mood and digestive function.
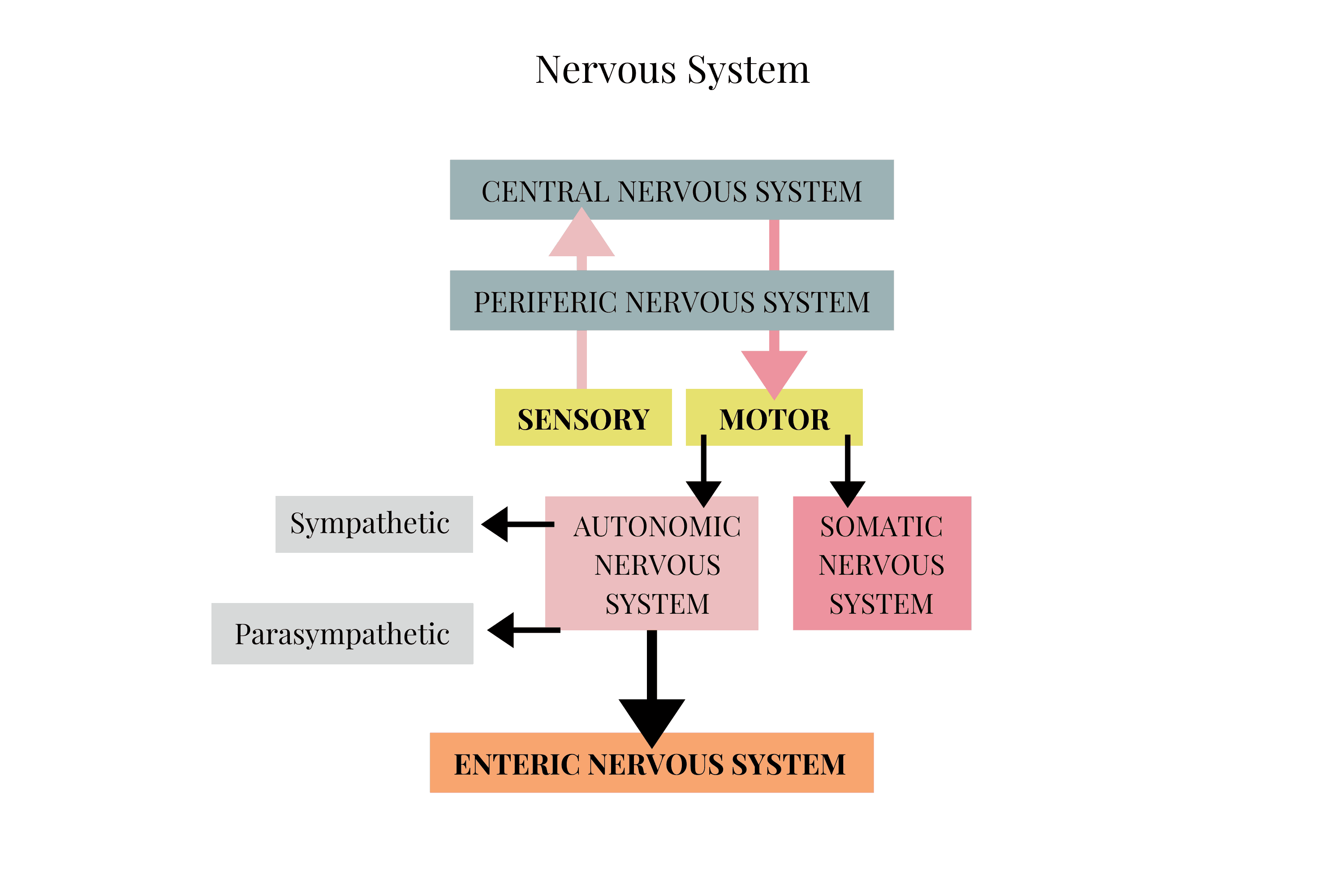
And there's definitely truth in it. Your Enteric Nervous System (ENS—the "rest and digest" system) is home to 500 million neurons in and around your gut.
While this number is staggering, it's only 0.5% of your body's total neuron estimate—with your brain comprising perhaps 100 billion neurons and a relatively modest 100 million in your spinal column.
Comparisons aside, your body's nerve cells are always talking to each other, providing invaluable real-time feedback about the innumerable interactions happening every moment—whether biochemical feedback loops or cell (and microbe) signalling.
Science is still figuring out precisely how it all works together. But there's also a lot we do know.
How do the signalling mechanisms between gut microbiota and brain actually work?
How Your Gut-Brain Connection Works
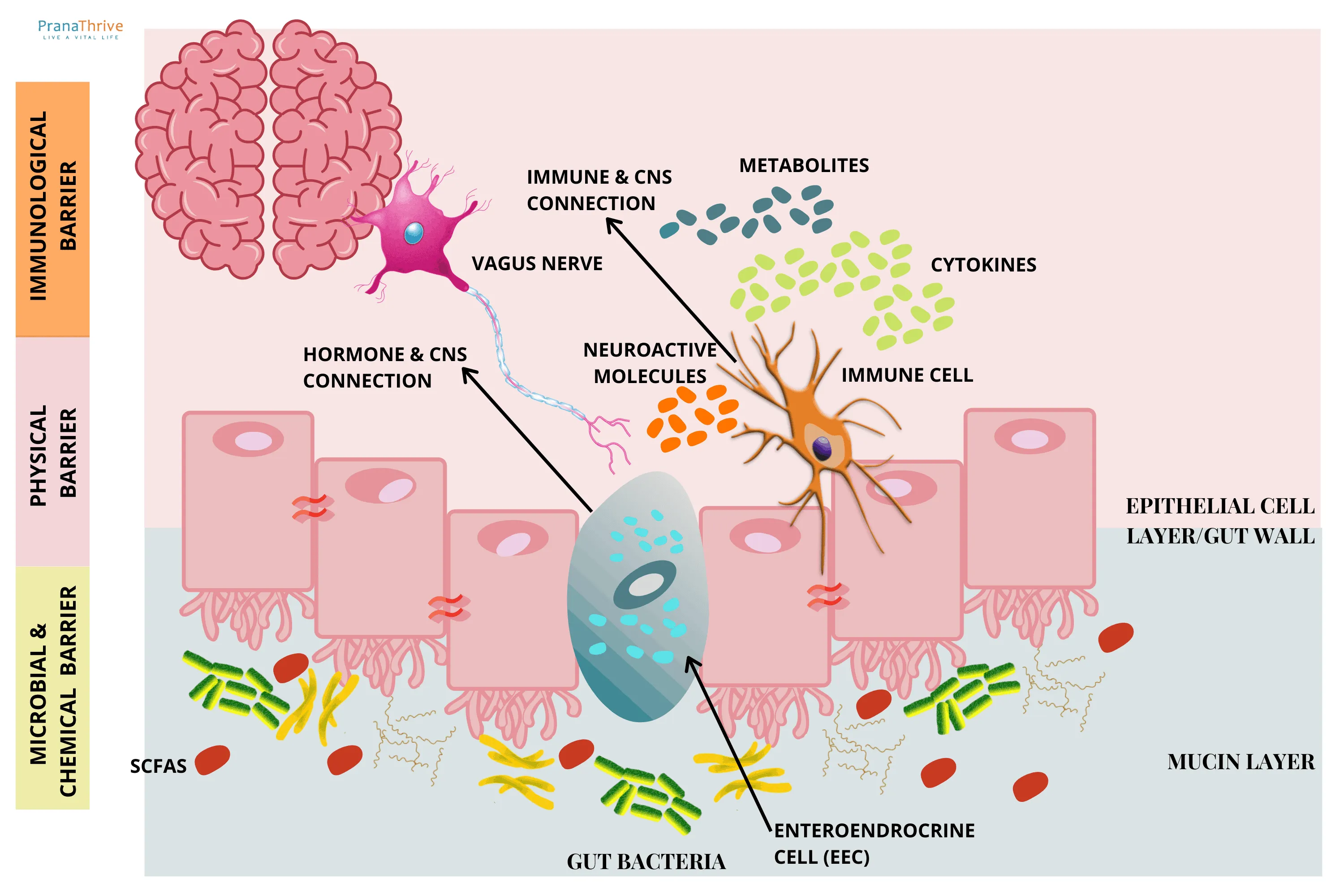
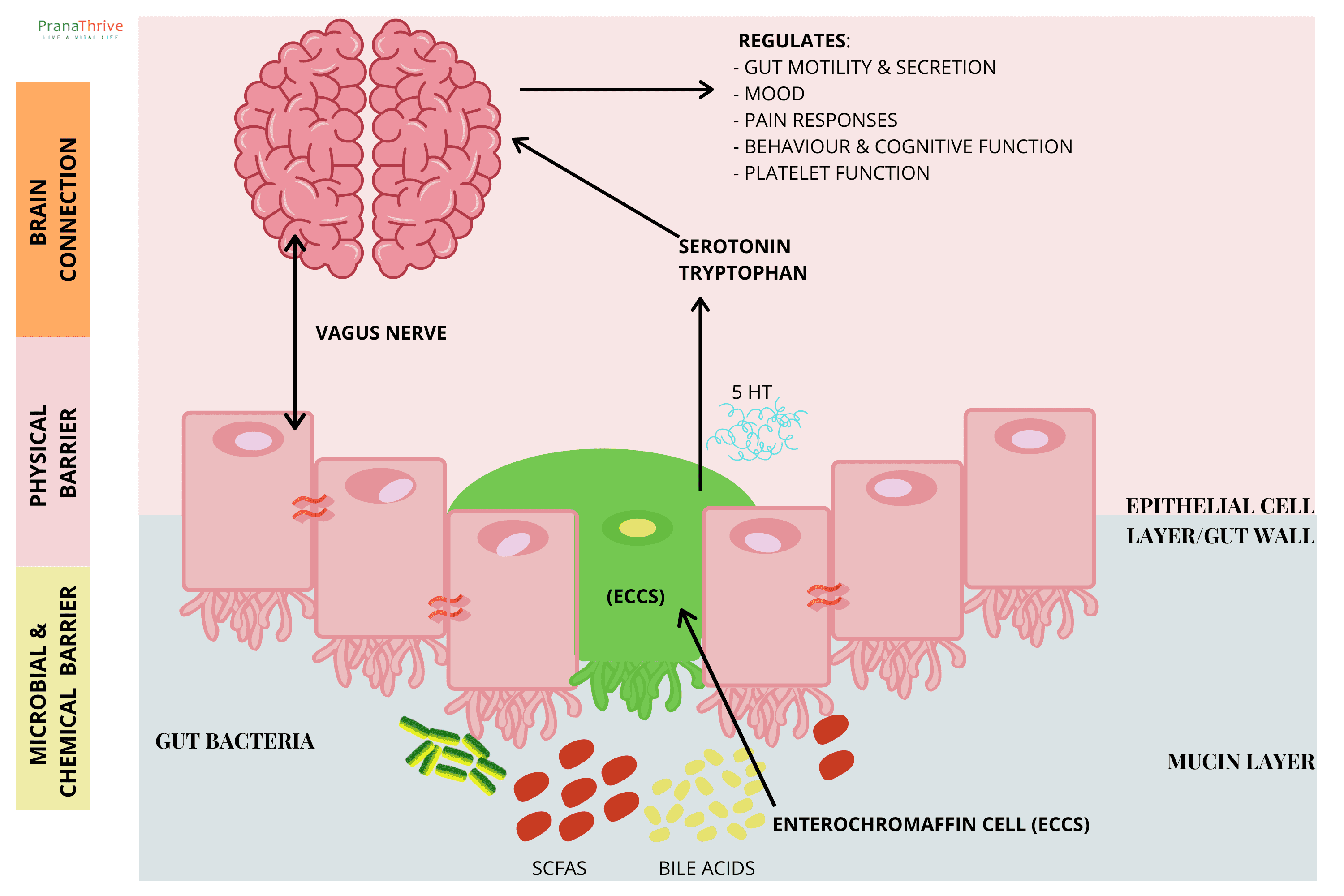
Current evidence suggests two main connection mechanisms about how the microbiome influences our brain and central nervous system (CNS):
Neuroimmune signalling pathways (immune and CNS connection)
Neuroendocrine signalling pathways (hormone and CNS connection)
Both of these mechanisms often involve the vagus nerve. And both need several microbial metabolites, including short-chain fatty acids (SCFAs), secondary bile acids (2BAs), and tryptophan (Trp).
These molecules then stimulate signals via interactions with specialised cells in the mucosal epithelial lining:
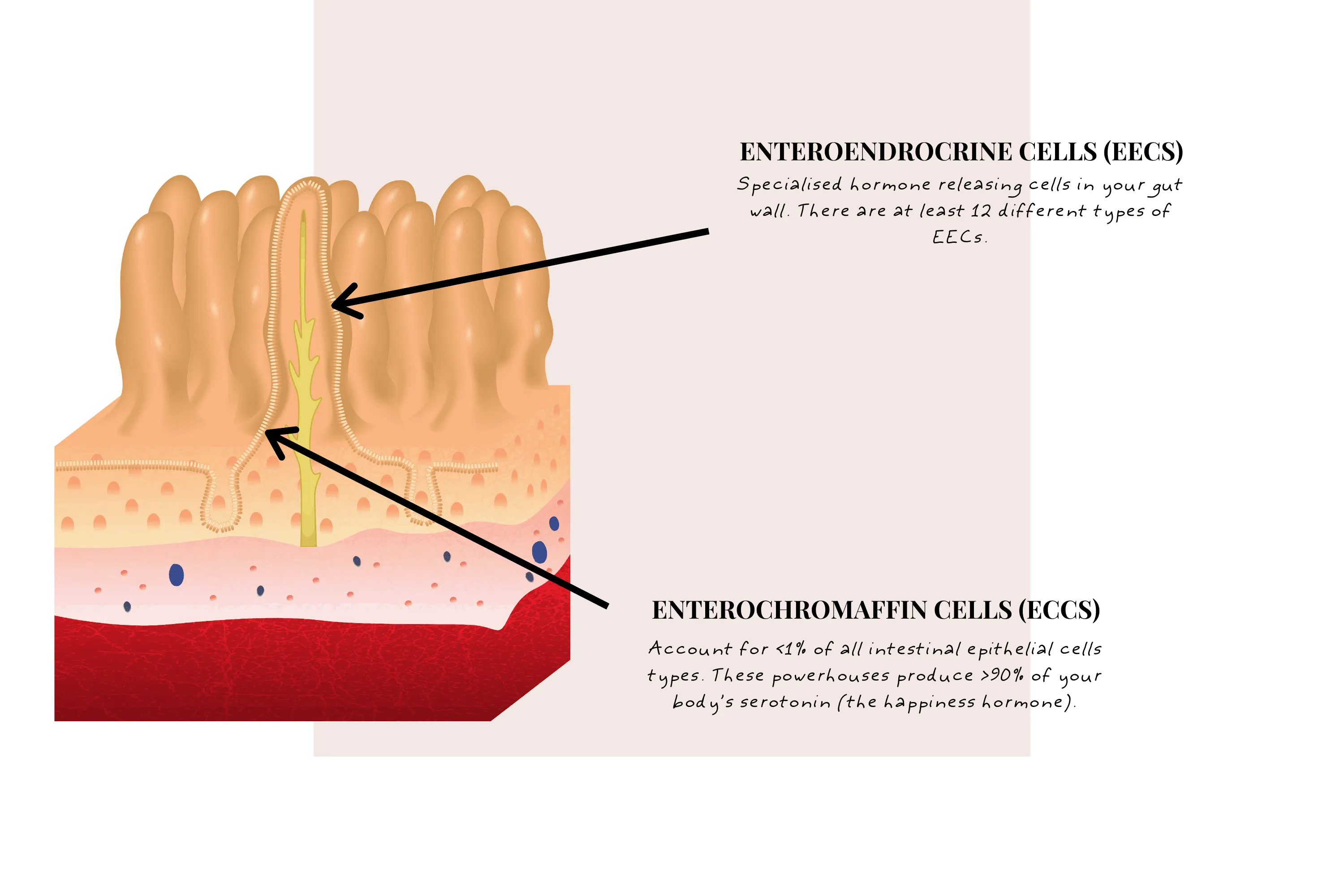
Enteroendocrine Cells (EECs)
Specialised hormone-releasing cells in your gut wall. There are at least 12 different types of EECs. Some processes EECs regulate include glucose levels, food intake, and stomach emptying.
Enterochromaffin Cells (ECCs)
Account for <1% of all intestinal epithelial cell types. These powerhouses produce >90% of your body's serotonin (the happiness hormone). They're thought to affect intestinal motility, secretion, nausea, and hypersensitivity.
Another GBA mechanism for SCFAs and other metabolites may be through direct transport—across the intestinal barrier and even the blood-brain barrier.
Interestingly, the microbiome can also activate CNS signalling by producing neuroactive molecules such as dopamine, norepinephrine, gamma-aminobutyric acid (GABA), and 5-HT (serotonin).
We'll talk more about each of these pathways as we go. But first, let's explore the vagus nerve.
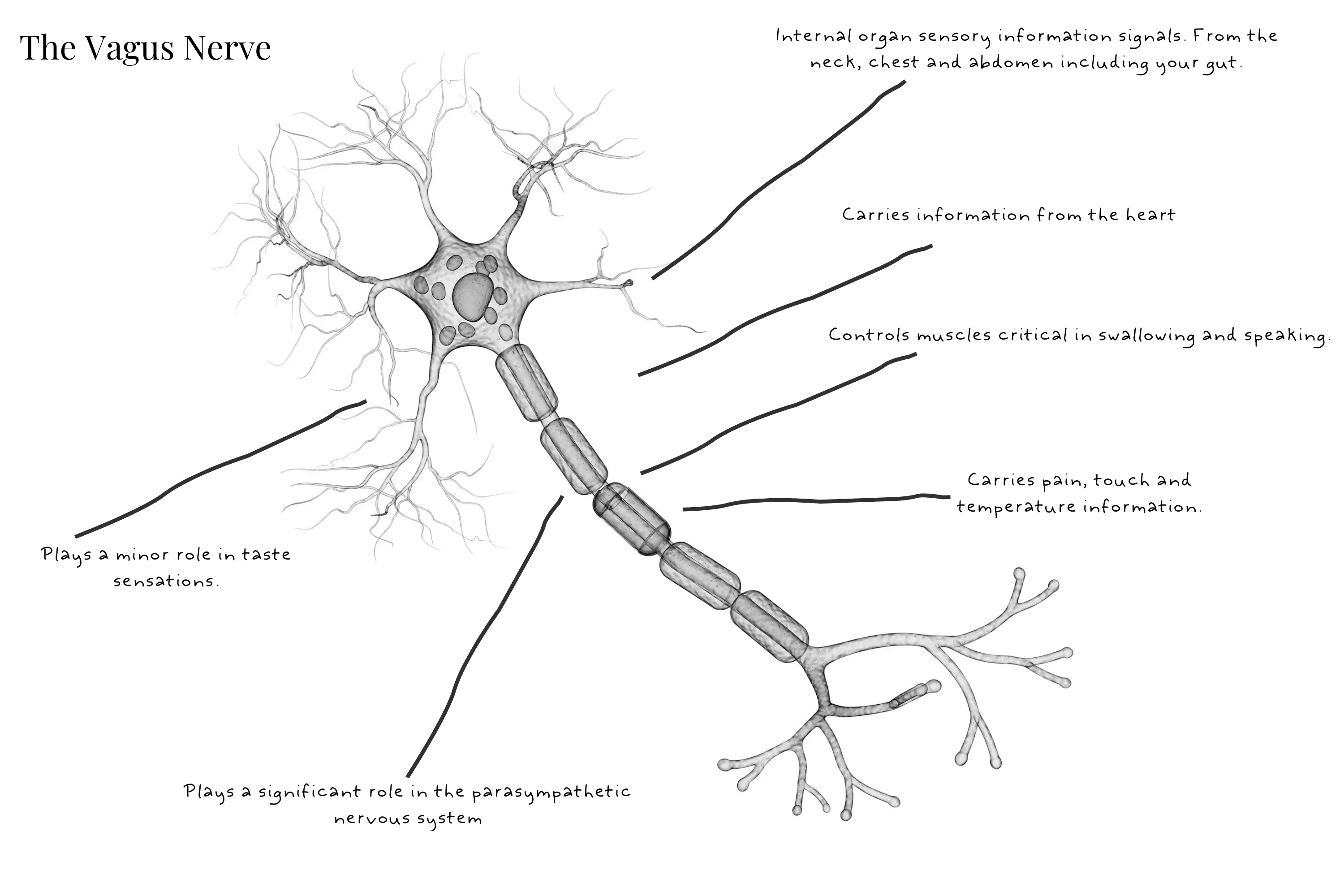
The Vagus Nerve
The vagus nerve, also known as cranial nerve X, is an extremely long nerve running from your brainstem to your colon.
It has many functions including:
Internal organ sensory information signals — From the neck, chest, and abdomen including your gut
Carries information from the heart — Including sensors that detect oxygen levels in the blood and blood pressure
Controls muscles critical in swallowing and speaking
Plays a significant role in the parasympathetic nervous system — Including "rest and digest" enteric nervous system functions and slowing of heart rate
Carries pain, touch, and temperature information — From the throat, ear, and meninges (brain membrane)
Plays a minor role in taste sensations — From the root of the tongue and epiglottis
As you can see, the vagus nerve plays a critical role in the gut and digestive process—top to bottom, from taste and swallowing through to digestion and excretion.
Understandably, if the vagus nerve is damaged, these many functions are negatively affected.
As a side note, the soothing effect of infant sucking occurs when pressure is applied to the soft palate, stimulating the vagus nerve and oxytocin production. Oxytocin has also been found to modulate serotonin release (remember our ECCs!).
In a nutshell: The vagus nerve acts as an information highway, both to and from the gut. It carries information from specialised cells, microbial metabolites, and other organ systems—and also influences many critical functions including digestion and associated intestinal epithelial immune and hormone signalling pathways.
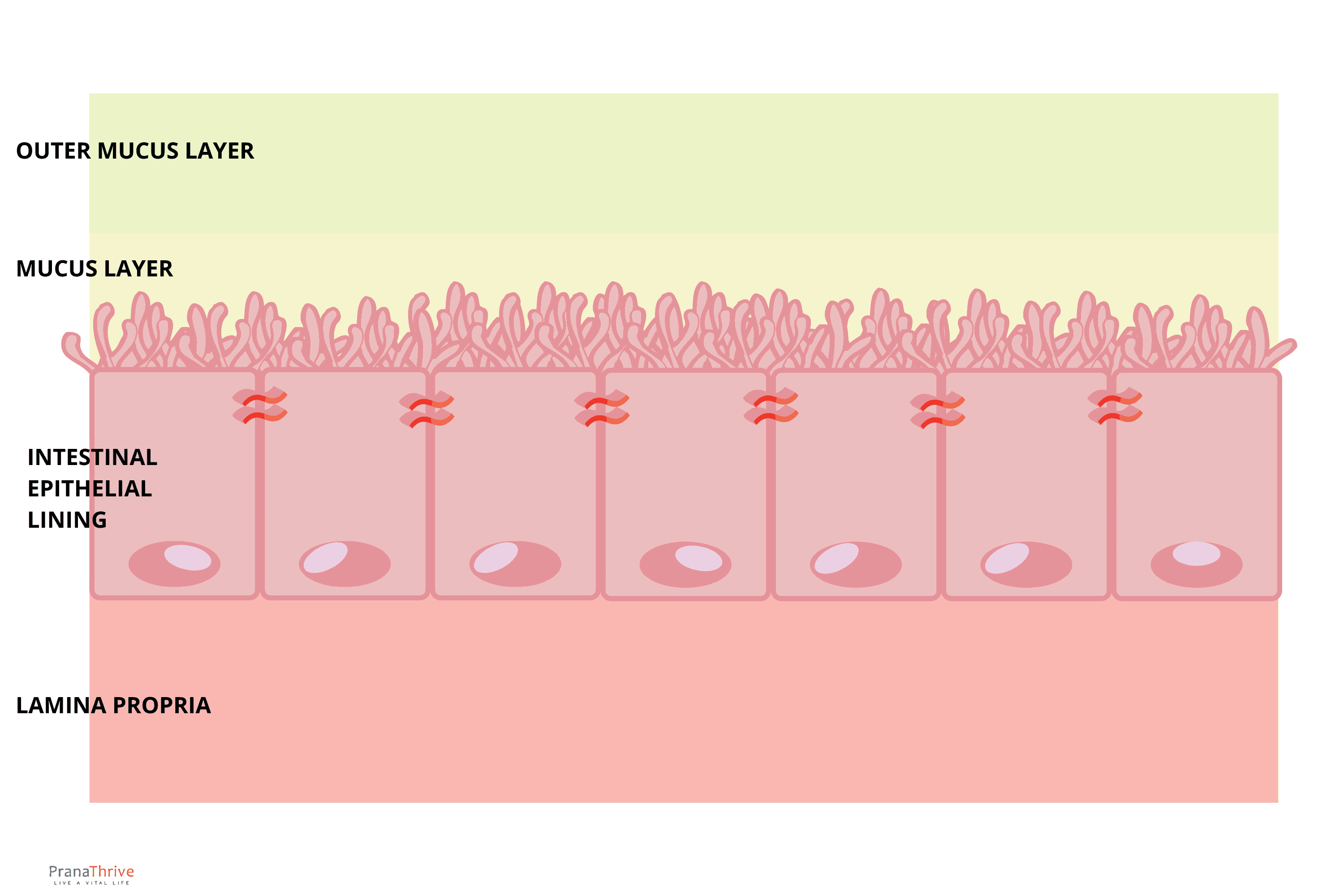
Intestinal Epithelial Lining—Your Intestinal Barrier
Your intestinal lining is a single cell layer thick. With its protective immunity-boosting IgA-rich mucus layer, it's all that stands between you and your food (and waste). Its integrity is foundational to your gut and overall health.
We've previously covered the importance of a healthy gut lining—here we'll briefly discuss its pivotal function.
Read more:
Your gut lining acts as a gatekeeper. Daily you expose it to all the food and drinks you consume (and microbial hitchhikers). It's the job of your intestinal barrier and associated cells to figure out who is welcome and who is not.
Your millions of gut lining neurons constantly relay information to your vagus nerve and through all your ENS nerve cells, all working to maintain a healthy and happy state of wellbeing.
However, it's important to understand what can affect it all. Gut microbes, stress, and inflammation can change your gut lining permeability—and the amount of information passing through our delicate intestinal barrier.
This means the amount of information reaching the brain from the gut is highly variable and dependent on you.
Stress and Leaky Gut
Stress causes epithelial defects (leaky gut) by two known mechanisms:
Direct influence on epithelial permeability
Alterations in intestinal mucosal layer
Both lead to increased transit of gut microbes and metabolites through the gut lining.
Escherichia coli (E. coli) is an important example. Its membrane lipopolysaccharide (LPS) promotes gut inflammation. LPS resides on the membrane of E. coli and other Gram-negative bacterial cell walls.
Receptors in the gut lining can also moderate inflammation, antimicrobials, and immune tolerance. Specific cell types act as triggers, releasing antibacterial factors. Microbes even help maintain gut integrity, supporting the tight junctions crucial to holding the intestinal barrier together.
Your intestinal barrier is a key player in the gut-brain connection.
The Blood-Brain Barrier (BBB)
The intestinal lining is the natural barrier to signalling within the gut and part of the gut-brain axis. So too is the blood-brain barrier (BBB), but for the brain.
It regulates molecular traffic between your blood and your cerebrospinal fluid (CSF)—the critical fluid surrounding your brain and spinal cord.
The BBB is highly influenced by stress, gut microbes, and inflammation—all affecting the amount of information passing through.
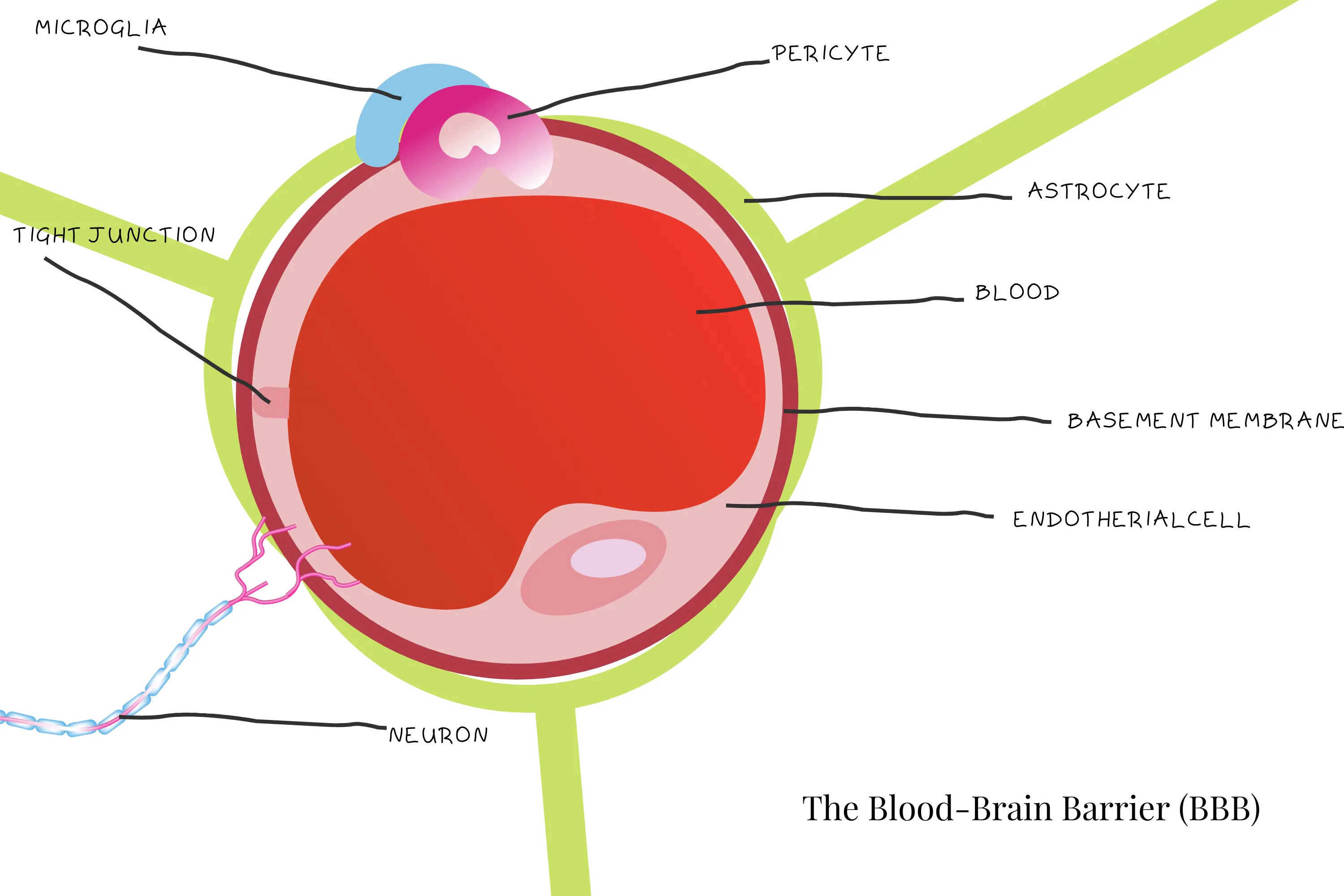
Gut microbes can influence this permeability because the BBB has tight junctions like your gut.
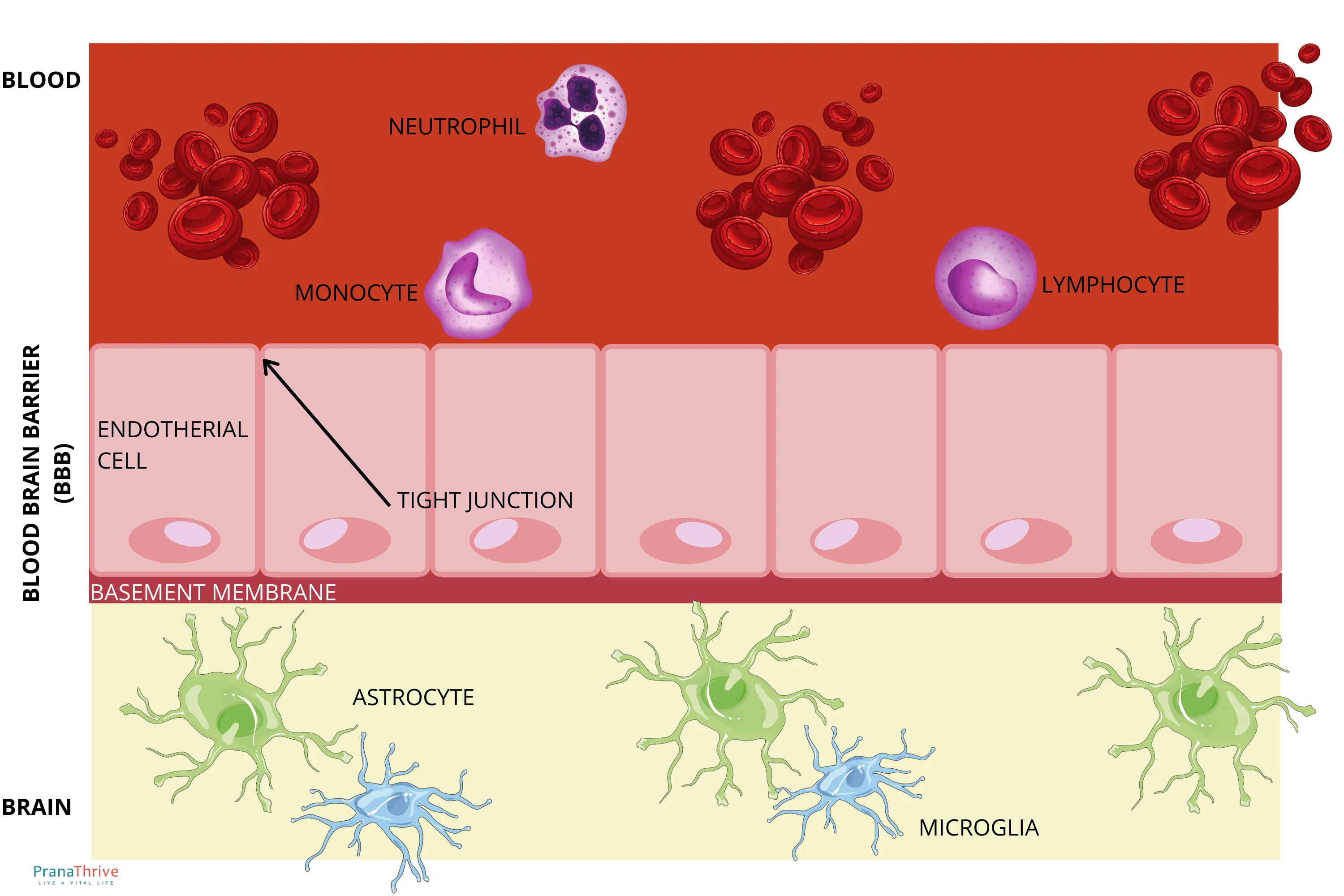
Science shows mice born without microbiomes ("germ-free") have more permeable (or open) barriers—both brain and gut. This permeability decreases (closes) with introduction of SCFA-producing bacteria. So SCFAs are thought to be critical in BBB development and maintenance.
We'll discuss SCFAs and the microbes that produce them in more detail shortly.
What's important to understand here? The connection between your microbiome, gut, and your brain is undeniable.
To help with this understanding, let's introduce the gut signalling mechanisms your body uses to communicate with your brain.
Gut Signalling Mechanisms
We've spoken about some of the mechanisms used in gut-brain signalling. Here we'll go into more detail.
The GBA signalling mechanisms may have complex names at first, so we'll explore them slowly to help you understand exactly how your gut and brain talk to each other.
1. Neuroendocrine and Enteroendocrine Signalling Pathways
These are important pathways where gut microbes communicate with endocrine cells in the gut. There are at least 12 types and numerous subtypes of gut endocrine cells. One of these we covered briefly above: enteroendocrine cells (EECs).
EECs contain and release greater than 20 types of molecules used in signalling. These molecules enter circulation and influence specific CNS centres—like those involved in ingestive behaviour—or even directly in the gut (or liver) to generate brain signals.
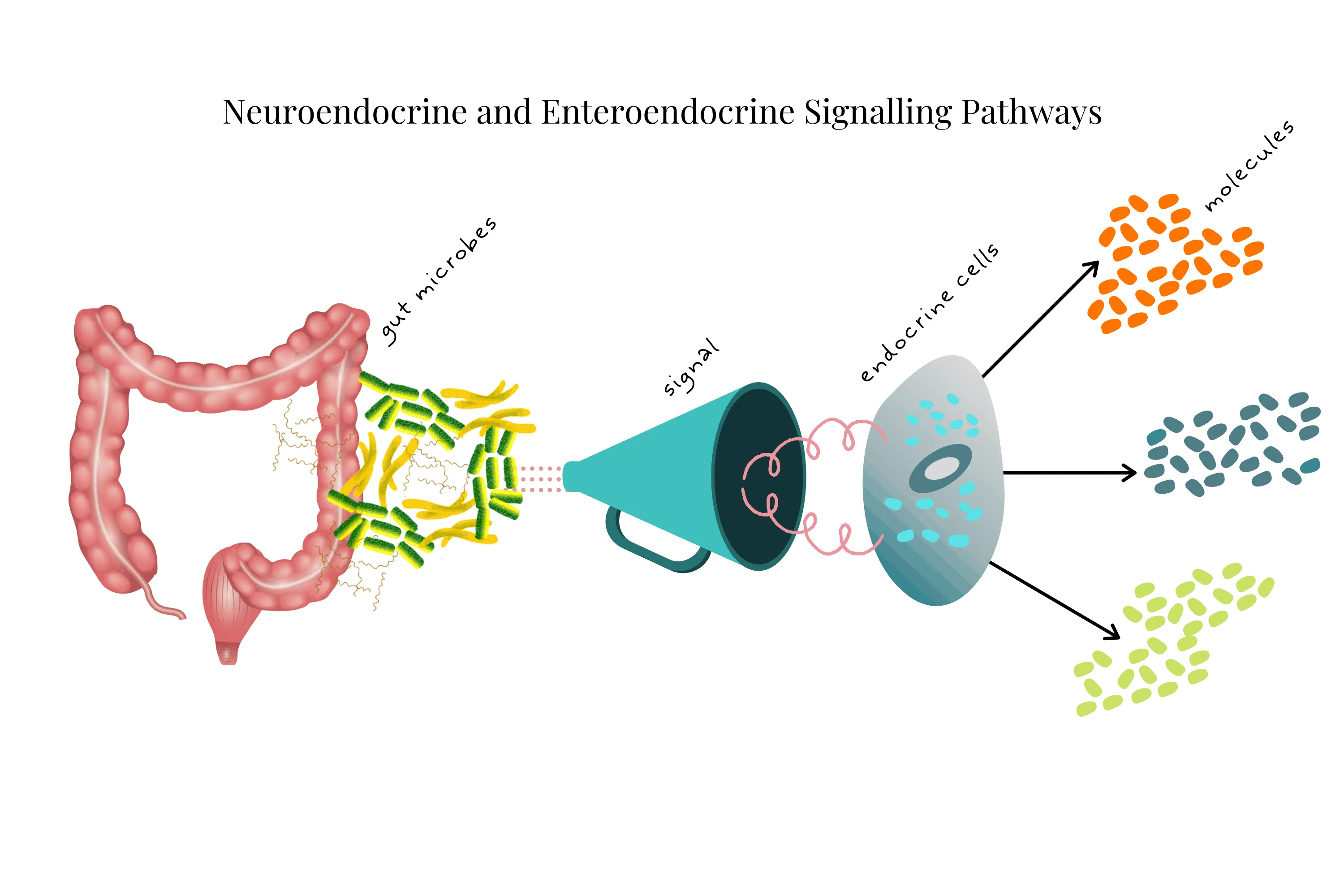
Short-Chain Fatty Acids (SCFAs) are major signalling molecules via EECs (and ECCs).
SCFAs are microbial fermentation products from resistant starch. They serve as important sources of energy, stimulate colonic blood flow, and stimulate cells responsible for secretion of factors like those which induce satiety (feeling full) and behaviour.
Specifically, acetate, butyrate, and propionate (common microbially derived SCFAs) regulate food intake and digestion via specialised receptors on EECs in the gut.
2. Enterochromaffin Cell (ECCs) Signalling
ECCs are a great example of two-way gut-brain communication.
A molecule called 5-HT (5-hydroxytryptamine—you may know it as the neurotransmitter serotonin) is produced and stored by ECCs in the gut. They stockpile more than 90% of the body's serotonin!
Serotonin regulates many functions:
Gut motility and secretion
Mood
Pain responses
Behaviour and cognitive function
Even platelet function
Incredibly, SCFAs and secondary bile acids (derived from spore-forming bacteria in the gut) regulate a large fraction of ECC serotonin synthesis and release.
The essential amino acid tryptophan (Trp) is the precursor to serotonin and many other important neuroendocrine signalling metabolites. Humans don't produce Trp, making it one of the "essential" amino acids needed in human diets.
Trp is used in serotonin synthesis. Gut microbes contribute to the availability of Trp in the blood through yet-to-be-confirmed pathways. However, Lactobacillus reuteri has been associated with Trp regulation.
Some common gut-colonising bacteria can even produce serotonin—like Streptococcus and Enterococcus sp. Escherichia coli is also known to produce serotonin, dopamine, and norepinephrine—all important mood regulators.
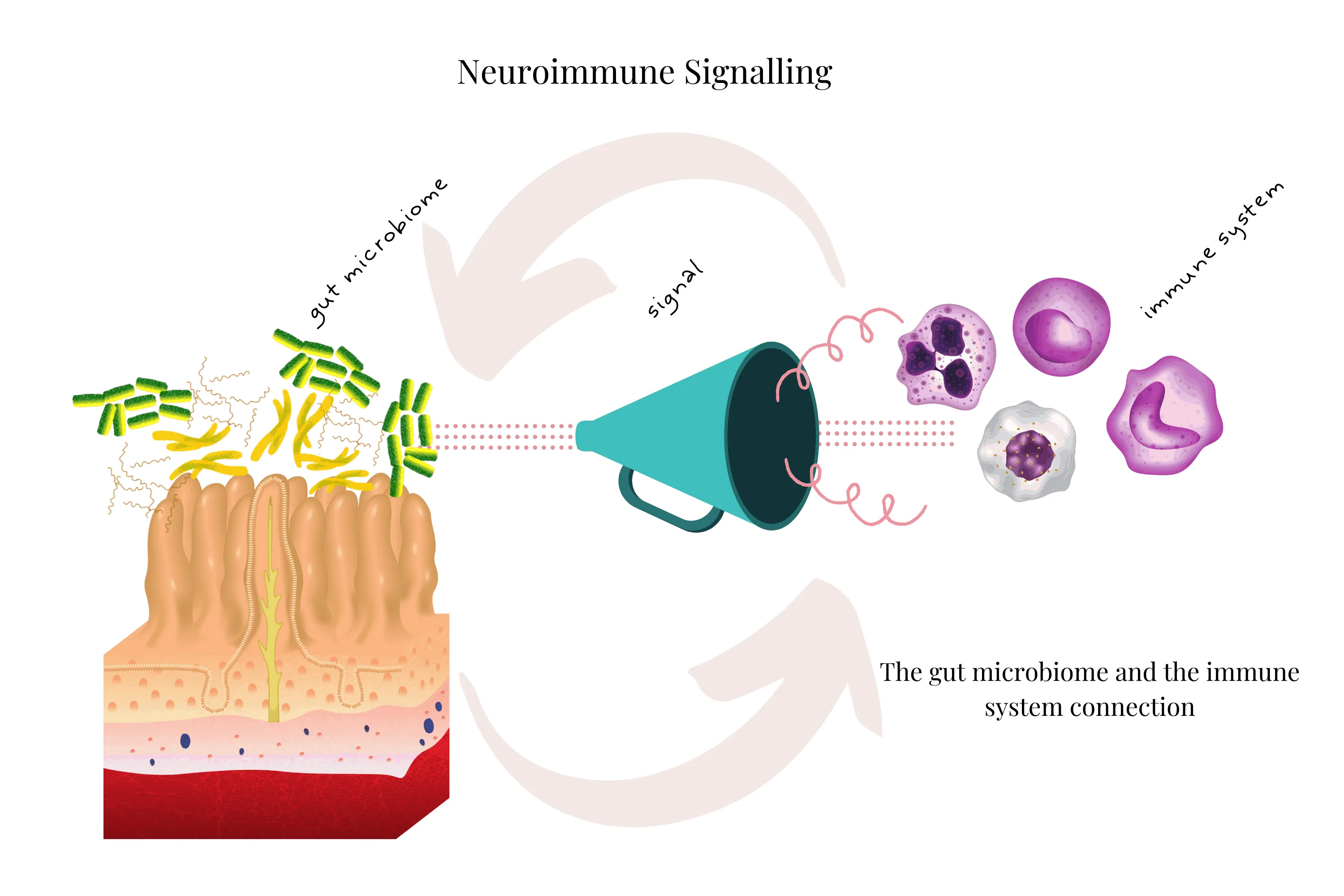
3. Neuroimmune Signalling
The gut microbiome and immune system connection has been researched extensively. There's much information around the direct link between gut microbes and immune response in CNS illnesses.
An interesting example is multiple sclerosis (MS)—a demyelination disease of the nerves that causes functional problems and stops cell-to-cell signalling, impairing motor function.
Imbalance or changes to gut microbiota are connected to MS, offering potential for treatment and management of this debilitating illness.
Microbes are also implicated in inflammation, autoimmunity, and immune cell trafficking.
In particular, Bacteroides fragilis (B. fragilis) can protect against demyelinating disease, as seen in experimental autoimmune encephalomyelitis (EAE). This is a common bacteria naturally found in the human gut.
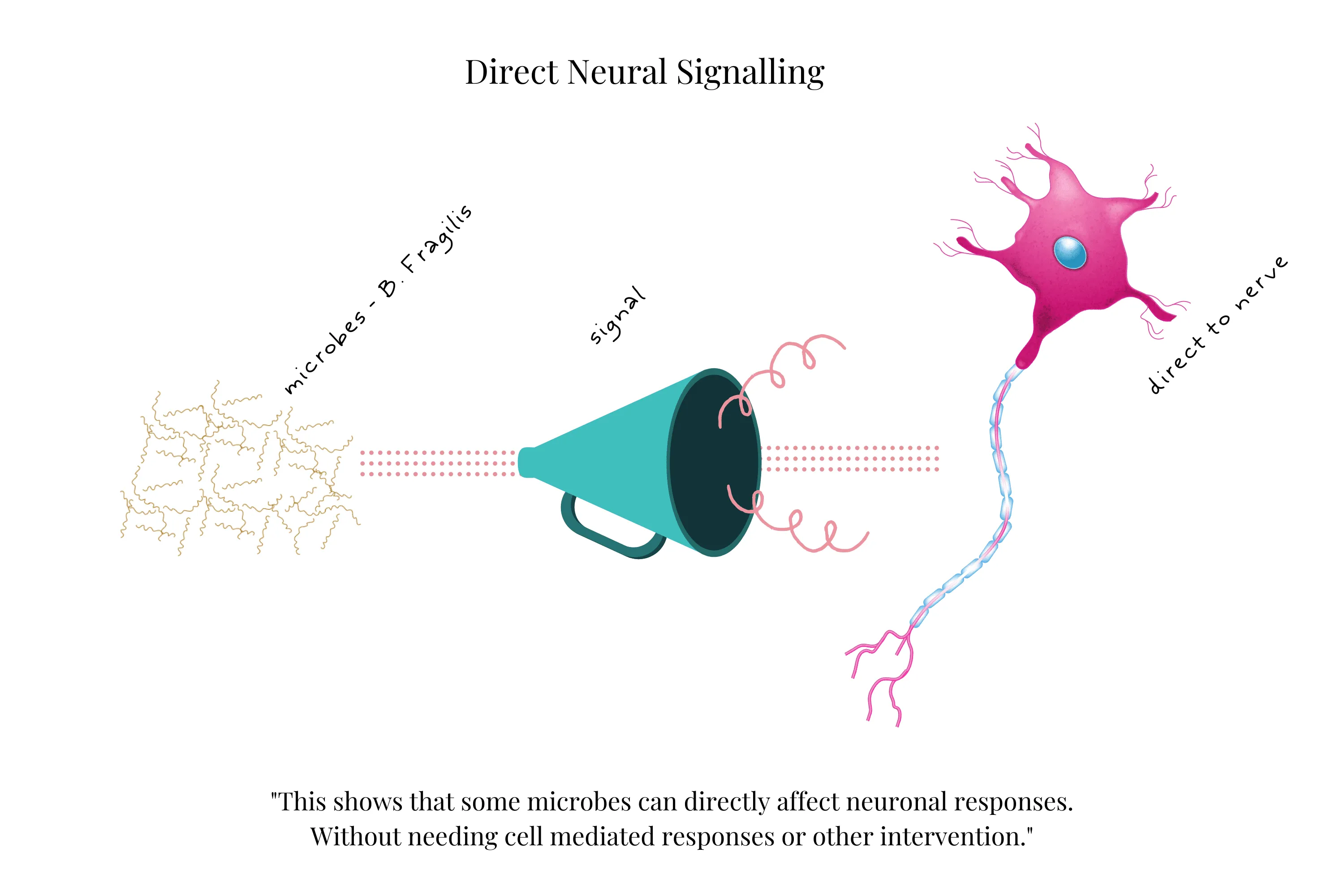
4. Direct Neural Signalling
Microbe-to-nerve-cell signalling can occur. B. fragilis has been implicated in direct activation of intestinal neurons. So too has Lactobacillus rhamnosus in polysaccharide A laboratory studies.
This shows that some microbes can directly affect neuronal responses without needing cell-mediated responses or other intervention.
There are also microbial metabolites that can affect neurons and their signalling.
Other Neurotransmitters Produced in Your Gut
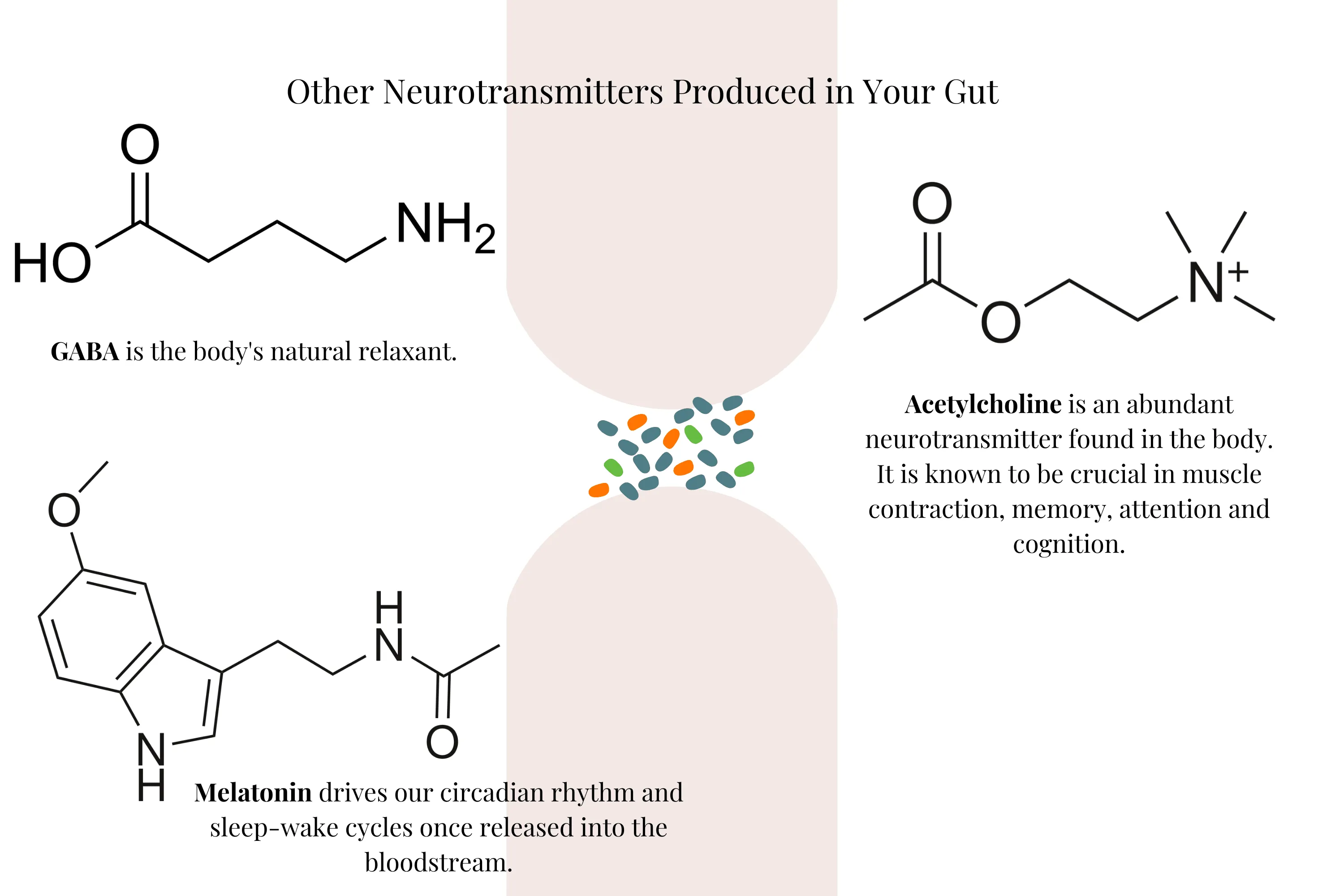
GABA (Gamma-Aminobutyric Acid)
GABA is the main CNS inhibitory neurotransmitter—the body's natural relaxant.
When GABA interacts with GABA receptors in neurons, it inhibits their action and blocks nerve impulses, creating a suppressing effect to oppose the excitatory effect of its precursor glutamate (another amino acid).
Interestingly, GABA is also produced by some gut bacteria. Bacteroides, Parabacteroides, Eubacterium, Bifidobacterium, and Escherichia sp all express GABA-producing pathways. Lactobacillus rhamnosus also produces GABA.
Acetylcholine
Another Lactobacillus species, Lactobacillus plantarum (found in sauerkraut), produces acetylcholine.
Acetylcholine is an abundant neurotransmitter found in the body, known to be crucial in muscle contraction, memory, attention, and cognition. Those suffering from Alzheimer's disease show severe depletion of acetylcholine.
Melatonin
Melatonin is produced by ECCs in the gut. L-tryptophan is a precursor for melatonin, reinforcing the importance of this essential amino acid.
Melatonin is also produced in the pineal gland. It drives our circadian rhythm and sleep-wake cycles once released into the bloodstream. Digestion and food intake are also regulated by this important endocrine hormone.
Enterobacter aerogenes (E. aerogenes) is a bacteria that colonises the human gut. It responds to melatonin and exhibits circadian growth patterns—meaning its growth pattern changes when exposed to melatonin. This supports the notion that non-algal microorganisms exhibit bacterial biological clocks.
Similarly, the human microbiome exhibits diurnal changes in both expression and abundance corresponding to feeding times and circadian cycles. Hence why shift workers and frequent flyers are more likely to suffer with dysbiosis and associated disease states.
The microbiome can recover with reinstated circadian and feeding cycles, showcasing the incredible ability of the microbiome to heal.
And we all know the importance of sleep for mental health.
Mental Health and Your Gut
There are many conditions linked with both gut and mental health. Here we'll briefly discuss only a few of the most common.
Inflammation and gut health are key in mental illness and associated disease states. Mental health is not only in your brain. If you believe you or anyone you know is suffering from these conditions, seek help.

Depression & Anxiety: Your Brain (and Gut) on Fire
Anxiety and depression often present together—and often with other gut conditions such as irritable bowel syndrome.
Feelings of helplessness, extreme irrational fears, and inability to cope with daily life are typical of depression and anxiety. Inflammation is a common trait for those suffering with depression.
Inflammation can alter brain signalling patterns and many other functions. Inflammatory conditions show an increased risk of depression—conditions such as diabetes, multiple sclerosis, and asthma.
Excitingly, evidence is mounting around specific microbial changes in common mental health conditions like depression.
There are an increasing number of studies showing positive results—specifically in modifying the intestinal microbiome with probiotic supplements to ease anxiety symptoms.
Autism Spectrum Disorder (ASD): A Rising Concern
Autism is a rapidly rising condition currently predominantly seen in children. Typical symptoms include difficulty in social situations, communication, and repetitive behaviours.
But so too, significant gut symptoms.
Children with ASD are at higher risk for general gastrointestinal complaints such as diarrhoea, constipation, and abdominal pain. The term "autistic enterocolitis" has been coined to describe these debilitating symptoms.
Anxiety and sensory symptoms are also common in this complex and multifaceted condition. While the cause is still unknown, there's mounting evidence implicating the gut microbiome and its role in normal development and function of the nervous system.
Microbiota transfer therapy (MTT) and faecal microbial transplant treatments can alleviate ASD symptoms. Bacterial diversity and relative abundance can change—in particular, common gut bacteria Prevotella and Bifidobacteria were seen to increase post-treatment.
Research such as this offers hope to families living with ASD. The once-thought "neurological" disease is a far more complex gut-brain connection syndrome.
IBS: Gut and Brain Irritation
Irritable bowel syndrome (IBS) is what's termed a functional intestinal disorder, where the function of the intestines is affected. Approximately 10–20% of the population worldwide suffer with IBS.
Typical IBS symptoms are varied but may include:
Abdominal pain
Bloating
Straining
Muscle aches
Urgency
Generally altered bowel habits
Most sufferers also report decreased quality of life.
A strong link exists between IBS and mental health—both depression and anxiety are common in those with IBS.
A number of studies report IBS patients as having significantly different microbiome communities compared with normal healthy patients. Some even show different brain volumes, suggesting a link between brain structure and microbiome structure.
This is an area where more research is needed. The exact cause is unknown. However, some natural treatments show promising results—such as those combining diet modification, pre- and probiotics, and lifestyle changes.
Book Your Free Evaluation Call
Understanding Your Gut-Brain Health
The science is clear: your gut microbiome profoundly affects your mood, anxiety, depression, and cognitive function through neurotransmitter production, SCFA synthesis, and immune signalling.
But here's what the research doesn't tell you: which bacterial species YOUR gut is missing.
Some people are severely depleted in Faecalibacterium prausnitzii (butyrate producer with anti-anxiety effects). Others are missing GABA-producing Bifidobacterium or Lactobacillus species. Some have elevated inflammatory bacteria producing LPS that triggers neuroinflammation.
Our AIM Method uses comprehensive testing to identify which neurotransmitter-producing bacteria are depleted, which inflammatory species are elevated, and which interventions will actually support YOUR gut-brain axis.
Book Your Free Evaluation Call
Power of the Microbiome
What this all shows us is how the microbiome has a massive effect on our brains. It influences everything we thought was "all in our heads"—from mood and behaviour to classical mental illnesses.
Ultimately, your thousands of gut microbial species form a complex ecology, feeding both each other and us with nutrients, vitamins, neurotransmitters, and metabolites critical for our wellbeing.
To this end, there's a new field of science called "psychobiotics"—investigating how powerful our gut bacteria can be, especially in influencing common mental conditions like depression and anxiety.
So with the microbiome playing such a huge role in our mental (and general) health, it makes sense to look after it.
Are you keen to understand your gut microbes better? A non-invasive comprehensive microbiome test can help. You'll learn exactly which microbes you have supporting your health—and which are missing.
Once you know what's going on in your gut, there are a number of simple changes you can make to positively influence your gut and mental health.
How to Improve Your Gut-Brain Health
Fix Your Gut First
Most gut healing advice follows a familiar phrase: "In case of emergency, put your own oxygen mask on first."
Similarly, you need to fix your gut lining first. Tighten those incredible tight junctions. Stem the flow of inflammation-causing food and microbes sneaking through your gut lining.
Healing (and sealing) your gut lining reduces the inflammatory cytokine cascade—a natural immune process wreaking havoc on your gut and brain.
Followed by seeding your gut with beneficial microbes, this is a powerful combination to start your journey back to health.
Step 1: Heal & Seal - Nourish and Nurture Your Gut with Diet
Reduce inflammation and support your brain health. Healing and sealing your gut is absolutely vital.
Some easy first steps are listed below. However, a personalised consultation with a qualified holistic practitioner may help. Support is key.
Eat whole foods. Cut out processed and packaged food-like substances laden with artificial sweeteners and chemically derived flavours, colours, and preservatives. These compounds negatively affect the microbiome and don't provide the nutrient building blocks needed for a healthy gut. They're also often difficult to digest and loaded with hidden sugars feeding yeasts like Candida, a common culprit in leaky gut.
Increase your liquids. Estimates vary, but it's commonly recognised that our bodies are 70–80% water, with digestion requiring up to 9L. Eating foods with higher water content can assist your digestive action and allow your gut to heal.
Drink more water. This is a simple and effective healing tool. Another easy way to increase your liquids is to gently cook your food with abundant water. Methods such as boiling and steaming provide much-needed hydration to your food and are an easy-to-digest alternative to raw foods, which can be tough on a damaged gut.
Supplement for healing. There are many easy-to-find supplements that support your liver to detox and your gut to heal. Some of these include L-glutamine, arabinogalactan, slippery elm, colostrum, DGL liquorice root, and quercetin. As always, it's helpful to work with a qualified practitioner when choosing supportive supplements.

Step 2: Seed - Build a Better Microbiome
Balance is key. What do we really mean by balance?
Microbiologists describe microbiota balance as being a combination of these factors:
Species richness — This describes the number of species in your gut. Species richness describes the dynamic balance keeping troublemakers in lower numbers.
Diversity — Diversity is the vast array of different types of microbiome inhabitants. It's a multicultural microbial community, describing their abundance relative to each other—beneficial versus non-beneficial microbes.
Essentially, you want lots of different types of microbes and lots of the beneficial health-supporting species—a rich and diverse ecology.
How? There are many easy and natural methods to boost or build a better microbiome:
Eat fermented foods. Naturally fermented (and non-pasteurised) sauerkraut, miso, kimchi, etc., contribute to gut flora diversity. Eating these foods every day is a great way to seed beneficial gut microbes. It needn't be expensive—you can easily make sauerkraut at home. If you're new to fermented foods, it's best to start small. Add a teaspoon of the fermenting liquid to your meals at first and build up to 1–2 tablespoons or more. Check in on how you feel and trust your gut.
Fill up on fibre. Fibre feeds the beneficial bacteria in your gut. Eating more fibre is an absolute must, non-negotiable step in gut seeding. You need to eat foods that feed all those good bugs, or they'll starve. Good sources of fibre include many vegetables like leafy greens, asparagus, carrots, artichokes, and radishes. Healthful fibre, including resistant starch, is often termed a prebiotic. Though you can now find prebiotic supplements, enjoying your fibre in whole foods is always best.
Take a good probiotic. Probiotic supplements are not all created equal. Finding a high-quality probiotic is key. These often include multiple strains and a high number of colony-forming units (CFUs), meaning you'll get more species richness and higher diversity. You'll receive a good dose of bacterial strains proven to be gut supportive. Some we've discussed are brain health-supportive. Check the label for L. plantarum (acetylcholine-producing) and Bifidobacteria (GABA-producing).

Step 3: Thrive—Build a Healthier Lifestyle
Building a lifestyle that supports your gut and mental health is so important.
Stress has been shown to affect the community structure of the microbiome for over 40 years. Relatively brief exposures to stress can change the microbiome significantly—in as little as 2 hours.
Similarly, stress while pregnant can alter infant outcomes, including microbiome profiles.
Reducing your exposure to psychological and emotional stress is essential. Physical stress also hinders your healing journey. Look out for stressors such as exposure to pesticides, chemicals, and electromagnetic stress.
Getting outside in nature is also paramount. Enjoying your family and friends provides innumerable benefits, including much-needed support and a healthy change for your microbiome.
When Diet & Lifestyle Aren't Enough: Why Testing Matters
You've been doing everything right. You've cut out processed foods, you're eating fermented foods daily, you've increased your fibre intake, and you're taking a high-quality probiotic. You're managing stress, getting outside, and prioritising sleep.
But you're still experiencing:
Anxiety or depression that won't lift
Brain fog and difficulty concentrating
Mood swings or irritability
Sleep issues despite good sleep hygiene
Persistent gut symptoms alongside mental health struggles
Here's what you need to understand: Diet and lifestyle can support a healthy gut-brain axis, but they can't always restore a severely imbalanced one.
Why Diet and Lifestyle Aren't Always Enough
1. You Don't Know Which Neurotransmitter-Producing Bacteria Are Missing
Eating fermented foods and taking probiotics provides beneficial bacteria—but only if you know which species you're actually depleted in.
If your Bifidobacterium (GABA producers) are adequate but your Faecalibacterium prausnitzii (butyrate producer) is severely depleted, generic probiotics won't address the root cause of your anxiety. You need targeted interventions that rebuild butyrate-producing species.
Without testing, you're guessing which bacterial species are missing.
2. Elevated Inflammatory Bacteria May Be Driving Neuroinflammation
You might be eating perfectly, but if you have elevated Klebsiella, Proteus, or Enterobacter (bacteria that produce inflammatory lipopolysaccharides), those organisms will continue triggering neuroinflammation regardless of your diet.
LPS crosses the blood-brain barrier and directly contributes to depression, anxiety, and cognitive decline. Dietary changes alone can't eliminate established bacterial overgrowths—you need targeted antimicrobials.
3. Your Gut Barrier May Be Severely Compromised
If you have significant intestinal permeability (leaky gut), eating anti-inflammatory foods helps—but healing the barrier requires more than diet. You need specific nutrients (L-glutamine, zinc carnosine, butyrate), targeted probiotics (Akkermansia muciniphila, Lactobacillus plantarum), and potentially elimination of foods triggering immune responses.
Without testing, you don't know if your gut barrier is compromised or which interventions will repair it most effectively.
4. You're Feeding the Wrong Bacteria
Not all fibre feeds beneficial bacteria. Some fibre types feed opportunistic bacteria instead of neurotransmitter producers.
If you're eating fibre that feeds inflammatory bacteria rather than Faecalibacterium or Bifidobacterium, you might actually make neuroinflammation worse. Testing reveals which species need support and which fibres to prioritise.
What Testing Reveals
When Victoria reviews comprehensive metagenomic test results, she identifies:
Depleted neurotransmitter-producing bacteria (Faecalibacterium, Bifidobacterium, Lactobacillus, serotonin producers)
Elevated inflammatory bacteria (Klebsiella, Proteus, Enterobacter, LPS producers)
Functional capacity (Is your microbiome producing butyrate? GABA? Serotonin? Metabolising tryptophan?)
Gut barrier integrity markers (Are inflammatory metabolites elevated?)
This information allows me to create a targeted protocol:
Specific antimicrobials for inflammatory bacterial overgrowths
Targeted probiotics for depleted neurotransmitter-producing species
Particular prebiotic fibres for your bacterial profile
Gut barrier repair protocols
Dietary modifications based on YOUR bacterial balance
The Bottom Line
If you've been eating well, taking probiotics, and managing stress for 3+ months and still have anxiety, depression, or brain fog—the problem isn't your effort. It's that you're working blind.
Testing shows exactly what's happening in your gut-brain axis, which bacterial species are missing, and which interventions will actually support your mental health.
Book Your Free Evaluation Call
Stop Guessing Which Bacteria Are Missing
The research shows gut bacteria produce neurotransmitters that affect mood, anxiety, and cognition. But which bacteria is YOUR gut missing?
Our AIM Method combines comprehensive metagenomic testing (reviewed by Victoria, our in-house microbiologist) with personalised protocols that target YOUR specific bacterial deficiencies affecting mental health.
We don't recommend generic probiotics or diet plans. We identify which neurotransmitter-producing bacteria you're depleted in and create targeted interventions.
Book a free 15-minute evaluation call to discuss your symptoms and whether testing could reveal which bacterial imbalances are affecting your mood and cognition.
Book Your Free Evaluation Call
Conclusion
The gut-brain axis is a very real and innately powerful connection affecting us all every day. The influence your microbiome has on your mental health is undeniable—a supportive relationship fundamental to wellbeing.
Many gut bacteria produce neurotransmitters responsible for neurological communication. They're fundamental to many brain functions.
Many mental health conditions have gut health ties, with ample evidence supporting this connection. But it's a rapidly evolving field, and new studies are being published daily.
While it's helpful to keep up with the science, there are fundamentals you need to know. You can make a difference to your brain and gut health every day with amazing results.
Simply changing to a whole-food, fibre-rich, healing diet has numerous health benefits and may assist with positive mental health.
You may also need to find the right support or take a comprehensive microbiome test. Both are powerful tools to use on your healing journey.
And remember: it's not all in your head. You can help your head by healing your gut.
Book Your Free Evaluation Call
Find Out Which Neurotransmitter-Producing Bacteria YOUR Gut Is Missing
Your gut bacteria produce serotonin, GABA, dopamine, acetylcholine, and melatonin—neurotransmitters critical for mood, anxiety, sleep, and cognition.
But eating fermented foods and taking generic probiotics without knowing your bacterial balance is guesswork.
At Prana Thrive, we use our AIM Method to identify which neurotransmitter-producing bacteria are depleted, which inflammatory bacteria are driving neuroinflammation, and which interventions will actually support YOUR gut-brain axis:
Analyse — Comprehensive metagenomic testing reveals your levels of Faecalibacterium prausnitzii (butyrate/anti-anxiety), Bifidobacterium (GABA), Lactobacillus (various neurotransmitters), serotonin producers, and inflammatory bacteria. Reviewed by Victoria (our in-house microbiologist) and me (after analysing over 2,000 microbiome tests).
Integrate — A personalised protocol designed for YOUR bacterial imbalances. If testing shows depleted Faecalibacterium, we focus on butyrate support. If testing shows low GABA-producers, we target Bifidobacterium and Lactobacillus species. If elevated inflammatory bacteria, we use targeted antimicrobials. Not generic gut health advice—targeted protocols based on your test results.
Monitor — Ongoing support with regular check-ins, protocol adjustments, and retesting to ensure your gut-brain axis is healing. We track your progress for 3–6 months until your mental health and gut symptoms improve.
This isn't guesswork. It's precision.
We've helped over 2,000 clients improve their mental health by identifying which bacterial species are missing—not which supplements have the best marketing.
Book a free 15-minute evaluation call to discuss your symptoms, mental health challenges, and whether comprehensive testing is right for you.
We work with a limited number of clients each month to ensure everyone receives personalised attention. If you're ready to stop guessing which bacteria you're missing and get real answers about your gut-brain axis, book your call now.
Book Your Free Evaluation Call
No pressure. No obligation. Just clarity on which bacterial imbalances are affecting your mood, anxiety, and cognition.

