The Gut-Skin Connection
The Real Science Behind Clear Skin from Within
Author:
Amanda Ledwith, BHSc Naturopathy
Last Updated:
20 Dec 2025
Reading Time:
XX min
Categories:
Gut Connections
gut-skin-connection
What You'll Learn
The gut-skin axis is a powerful two-way communication system between your digestive system and your skin. When your gut microbiome is imbalanced, it triggers systemic inflammation that shows up as chronic skin conditions—psoriasis, eczema, acne, rosacea, and unexplained rashes.
How the gut-skin connection works:
Intestinal permeability (leaky gut) — When gut barrier breaks down, toxins and bacteria enter bloodstream, triggering immune reactions that manifest as skin inflammation
Microbiome imbalances — Depleted beneficial bacteria (Faecalibacterium prausnitzii, Akkermansia muciniphila) and elevated inflammatory bacteria (Proteobacteria, Streptococcus) drive systemic inflammation
Immune dysregulation — 70% of immune system located in gut; when gut bacteria imbalanced, immune system overreacts, causing skin flares
Stress-gut-skin feedback loop — Chronic stress disrupts gut flora, worsening skin conditions
Common skin conditions linked to gut dysfunction:
Psoriasis (often with IBS symptoms, depleted anti-inflammatory bacteria)
Eczema and atopic dermatitis (low microbial diversity, food intolerances)
Acne and rosacea (SIBO patterns, elevated Streptococcus, dietary triggers)
Chronic hives and urticaria (histamine intolerance, leaky gut)
Sensitive skin and chronic dryness (impaired gut barrier, nutrient malabsorption)
But here's what most people don't realise: You can eat clean, use gentle skincare products, and manage stress—but if you don't know which bacterial species are depleted or which inflammatory bacteria are elevated, you're treating symptoms, not root causes. Testing reveals whether you're missing Akkermansia (barrier integrity), depleted in Faecalibacterium (anti-inflammatory), or have histamine-producing bacteria driving skin inflammation.
Introduction
If you've ever wondered why skin creams only go so far—or why your eczema, acne, or psoriasis keeps flaring up—you're not alone. We've helped hundreds of clients conquer their chronic skin conditions. Now, science is finally catching up with what many holistic practitioners have long observed—there is a gut-skin connection. The health of your skin is a reflection of your gut health.
A wonderful example of this is Brendan's story.
When he first came to us in 2024, his hands and elbows were raw, cracked, and bleeding from years of relentless psoriasis. He'd tried every ointment and steroid under the sun, but nothing lasted. What finally changed things wasn't another cream—but a radical reset of his gut. In six months, his psoriasis was 80% gone.
And there are many more like him, living either entirely flare-free or still working their way to clear skin.
Helping people heal their inflammatory skin conditions is actually one of Amanda's specialities. After analysing over 2,000 microbiome tests, she's identified consistent bacterial patterns in clients with chronic skin issues—and created targeted protocols that address root causes, not just surface symptoms.
She has helped so many people heal their acne, eczema, psoriasis, dermatitis, rosacea, urticaria, and even just dry itchy skin—by looking at their gut microbiome, creating a personalised holistic plan, and working together to shift into gut-friendly lifestyle patterns.
This is the hidden story behind so many chronic skin issues.
Whether it's breakouts, rashes, or persistent dryness, your skin is constantly in conversation with the trillions of microbes and immune messengers inside your gut. And when this gut-skin conversation breaks down, the result isn't just a rash—it's a sign that something deeper needs attention.
In this article, we'll unpack the real science behind the gut-skin axis, show you what conventional advice often misses, and explain how personalising your approach—sometimes in ways that feel counterintuitive—can unlock real, lasting skin healing.
The Gut-Skin Axis: What Science Now Reveals
It's easy to think of skin problems as just "surface issues," but the real story runs far deeper—right down to the complex world of your gut microbiome.
In the last decade, researchers have mapped a powerful two-way communication network between your digestive tract and your skin, often called the gut-skin axis.
Here's what's going on under the surface:
1. Your Gut Lining Is Your Internal Skin
Just as your skin acts as a barrier to keep the outside world at bay, your gut lining is a boundary between your inner world and everything you swallow. When this barrier breaks down (a process called "leaky gut" in functional medicine, or increased intestinal permeability in research), toxins, bacteria, and undigested food particles can slip into the bloodstream.
Your immune system sees these as threats—and the fallout often shows up in your skin as inflammation, rashes, breakouts, or chronic conditions like psoriasis and eczema.
Read more: Do You Have Leaky Gut? (Plus Warning Signs to Look For)
2. The Microbiome Is Your Skin's Hidden Partner
Inside your gut, trillions of microbes are working behind the scenes—producing vitamins, regulating immune signals, and even creating anti-inflammatory compounds called short-chain fatty acids (SCFAs).
When your gut microbiome is balanced and thriving, these beneficial bacteria help calm skin inflammation and reinforce your skin's barrier. But when the gut ecosystem becomes imbalanced (a state known as dysbiosis), it can send a steady stream of inflammatory messengers to the skin.
Read more: What Is Gut Dysbiosis?
3. The Immune Conversation
Nearly 70% of your immune system is located along the gut wall. When your gut microbes are out of balance, your immune system can go into overdrive—triggering skin flares or even autoimmunity. Certain immune signals, like interleukin-17 (IL-17) or tumour necrosis factor-alpha (TNF-α), are now directly linked to both gut and skin inflammation in research.
This means that gut healing isn't just about what you eat, but also about how your immune system is trained by your microbes.
Read more: The Gut-Immune System Connection
4. The Feedback Loop – Stress, Sleep, and Skin
The gut-skin conversation doesn't happen in a vacuum. Stress, sleep deprivation, even what you put on your skin can change your gut flora—and your gut, in turn, influences how you respond to stress. This feedback loop is why chronic skin conditions so often flare after periods of emotional or physical stress, poor sleep, or even dietary slip-ups.
The bottom line?
If you want lasting skin health, you need to look beyond the surface and address root causes inside the gut. Topical treatments can provide some relief (but not always), but for real change, the solution is an inside job.
Common Skin Conditions with Microbiome Links
Every day, we see clear patterns between gut dysfunction and specific skin issues. Whether it's a high pathogen, LPS-dominant profile, or high histamine and low beneficial species, we've seen it all.
Many of the skin concerns below are now seen as autoimmune conditions, which also have microbiome links. Here's what often appears when the gut-skin axis is out of balance:
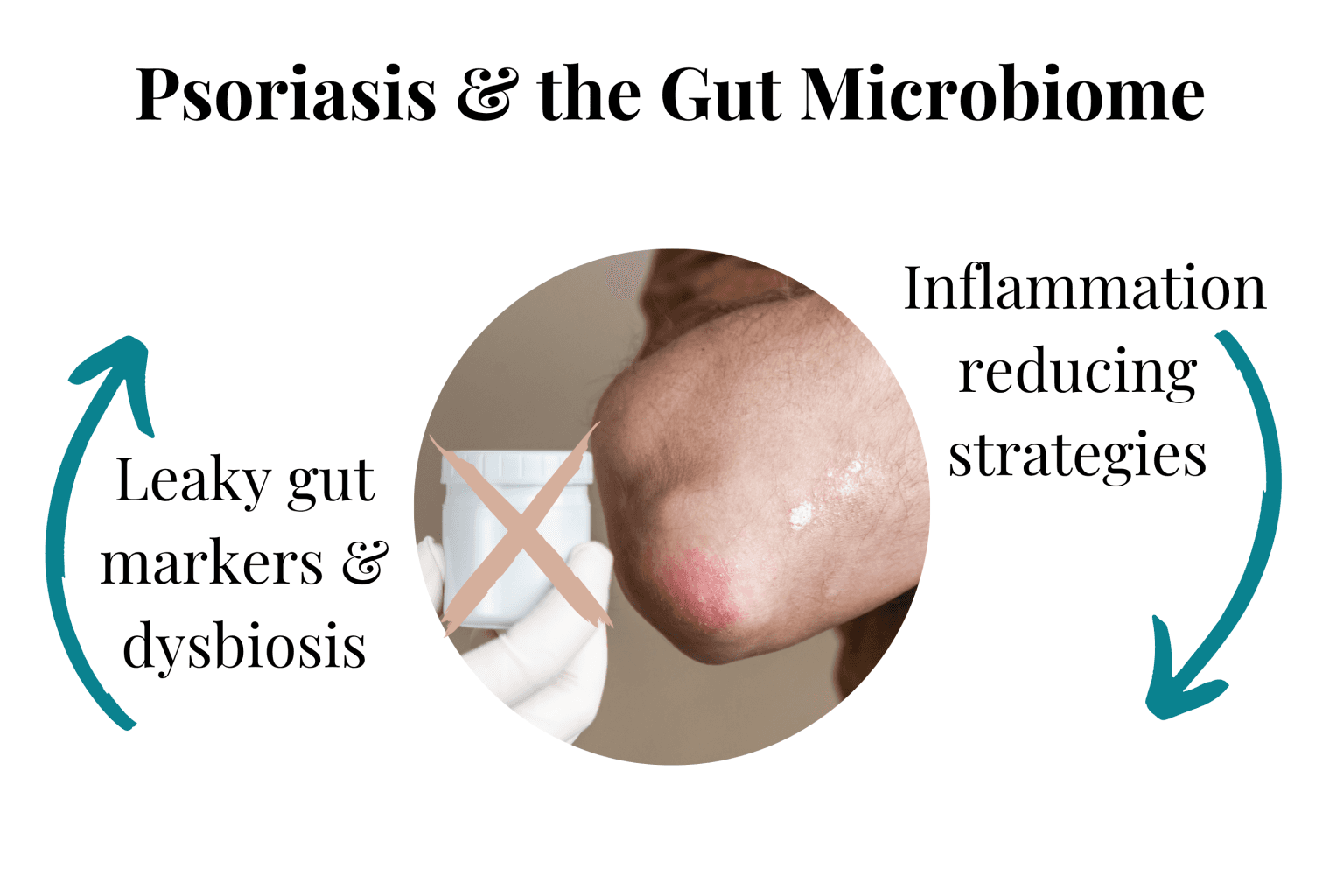
Psoriasis That Resists Standard Treatment
Many people with chronic plaque psoriasis have a long history of gut troubles—diarrhoea, bloating, or irritable bowel symptoms—that predate or flare alongside their skin outbreaks.
Research consistently links psoriasis with increased intestinal permeability and distinctive shifts in the gut microbiome, including lower levels of anti-inflammatory bacteria like Faecalibacterium prausnitzii and Akkermansia muciniphila.
Eczema and Atopic Dermatitis
These often go hand-in-hand with food intolerances, unexplained digestive symptoms, or early-life antibiotic use. Gut dysbiosis can drive overactive immune responses, leading to the chronic itch-scratch cycle.
Studies show that children and adults with eczema frequently have less microbial diversity, lower important probiotic species like Bifidobacterium, and higher levels of certain gut-derived inflammatory mediators.
Acne and Rosacea
Persistent, cystic acne that doesn't improve with topical regimens can be a red flag for underlying gut imbalances—especially small intestinal bacterial overgrowth (SIBO), high-sugar diets, or sensitivity to dairy and gluten.
Streptococcus is frequently high in chronic acne clients, while rosacea is linked with gut bacteria present in SIBO patterns.
Unexplained Rashes, Hives, or Urticaria
Chronic hives or recurrent rashes may signal a histamine intolerance or "leaky gut" allowing food proteins to trigger immune reactions.
We often see these symptoms in people with a long antibiotic history, unresolved gut infections, or high levels of hydrogen sulphide-producing bacteria.
Read more: Histamine Intolerance and Your Gut
"Sensitive Skin" and Chronic Dryness
For some, skin isn't visibly inflamed but is reactive, sensitive to products, or chronically dry and extremely itchy.
This can also be an external sign of impaired gut lining integrity, low short-chain fatty acids, or even malabsorption of key skin nutrients due to gut inflammation.
What do these patterns have in common?
The skin is rarely the first system affected, but it's often the loudest messenger. The real roots—microbiome imbalances, immune dysregulation, increased intestinal permeability—often simmer quietly for years before skin symptoms appear.
CASE STUDY
Brendan's Psoriasis, Gut, and the Power of a Microbial Reset
Brendan (who we talked about earlier) was 53 when he first came to see us, worn down by years of relentless skin and gut symptoms.
As a roof plumber running his own business, he was used to pushing through discomfort. But his psoriasis had become unmanageable—painful plaques on his hands, elbows, and knees cracked and bled with the slightest movement. Some nights, showering was unbearable; most days, the fatigue was like walking through wet concrete.
His doctors had tried every standard treatment: steroid creams, light therapy, even immune-modulating drugs. The skin would clear for a while, only to flare up again, each time worse than before.
But what Brendan didn't realise was how intertwined his symptoms really were. Alongside the skin pain, he lived with daily gut chaos—six to eight bouts of urgent diarrhoea, constant bloating, a thick feeling in his throat after meals, restless legs at night, and a persistent "foggy" brain that left him struggling to focus by mid-afternoon.
He was so used to powering through, he'd almost forgotten what it felt like to feel well.
Brendan's case was a classic example of the gut-skin axis in crisis:
Comprehensive stool testing revealed pronounced dysbiosis: low Faecalibacterium (an anti-inflammatory keystone species), high Proteobacteria (often linked to gut inflammation), and signs of increased intestinal permeability.
Markers of systemic inflammation were elevated. His diet, while seemingly "healthy" (although he did need to reduce his daily alcohol intake), was high in processed wheat and low in fermentable fibre.
His history included childhood antibiotics, a decade of stress and broken sleep, and years of relying on topical steroid creams.
Instead of chasing the next cream, Brendan embarked on a protocol focused on rebuilding his gut barrier, restoring microbial balance, and calming systemic inflammation. This included a gentle, low-reactivity gut repair diet; targeted prebiotics and postbiotics; stress management techniques; and careful, stepwise reintroduction of foods and probiotics. For the first time, the approach was "inside-out."
The Results
Within three months, Brendan's gut symptoms—once daily hurdles—became rare. His skin plaques softened, bled less, and for the first time in years, healing outpaced the flares. He described his thinking as "clearer than it's been in a decade." And even without retesting his microbiome, we saw dramatic improvement in his energy—he no longer suffered from afternoon crashes and returned to training in the gym.
Where he was previously flat, anxious, and withdrawn, he started to feel more physically confident, stable, and was even sleeping better.
Brendan's story isn't unusual.
It's a testament to the power of personalisation and the importance of treating the root, not just the rash. The gut-skin connection is real, profound, and—when you know where to look—full of hope for those who feel stuck.
Book Your Free Evaluation Call
Stop Treating Symptoms – Address the Root Cause
Your skin is a mirror of your gut. Chronic skin conditions like psoriasis, eczema, and acne are rarely "just skin issues"—they're signals of gut microbiome imbalances, intestinal permeability, and systemic inflammation.
Our AIM Method uses comprehensive metagenomic testing to identify which bacterial species are depleted (Faecalibacterium, Akkermansia), which inflammatory bacteria are elevated (Proteobacteria, Streptococcus), and which interventions will restore gut-skin balance.
We don't recommend generic gut protocols or elimination diets. We identify YOUR specific bacterial imbalances driving skin inflammation.
Book Your Free Evaluation Call
Gut Health and Psoriasis
Psoriasis is an inflammatory skin disorder that causes a rapid buildup of skin cells on your skin's surface. Psoriasis affects up to 11% of people in developed countries.
Just like eczema, psoriasis is caused by an overactive immune system, linked with gut dysbiosis. It causes an imbalance in your immune system that leads to widespread inflammation extending to your skin.
What is the evidence for this?
Patients who have psoriatic arthritis (a form of psoriasis) suffer from gut inflammation and are more likely to develop inflammatory bowel disease (IBD). In fact, up to 11% of patients with IBD have psoriasis.
Further evidence for the role of gut dysbiosis in the development of psoriasis is demonstrated by the fact that IBD patients and psoriasis patients have similar patterns of gut dysbiosis.
They have less beneficial bacteria—Bifidobacterium, Lactobacillus, and Faecalibacterium prausnitzii—and more pathobiont (beneficial) bacteria—Salmonella, Escherichia coli, Campylobacter, etc.
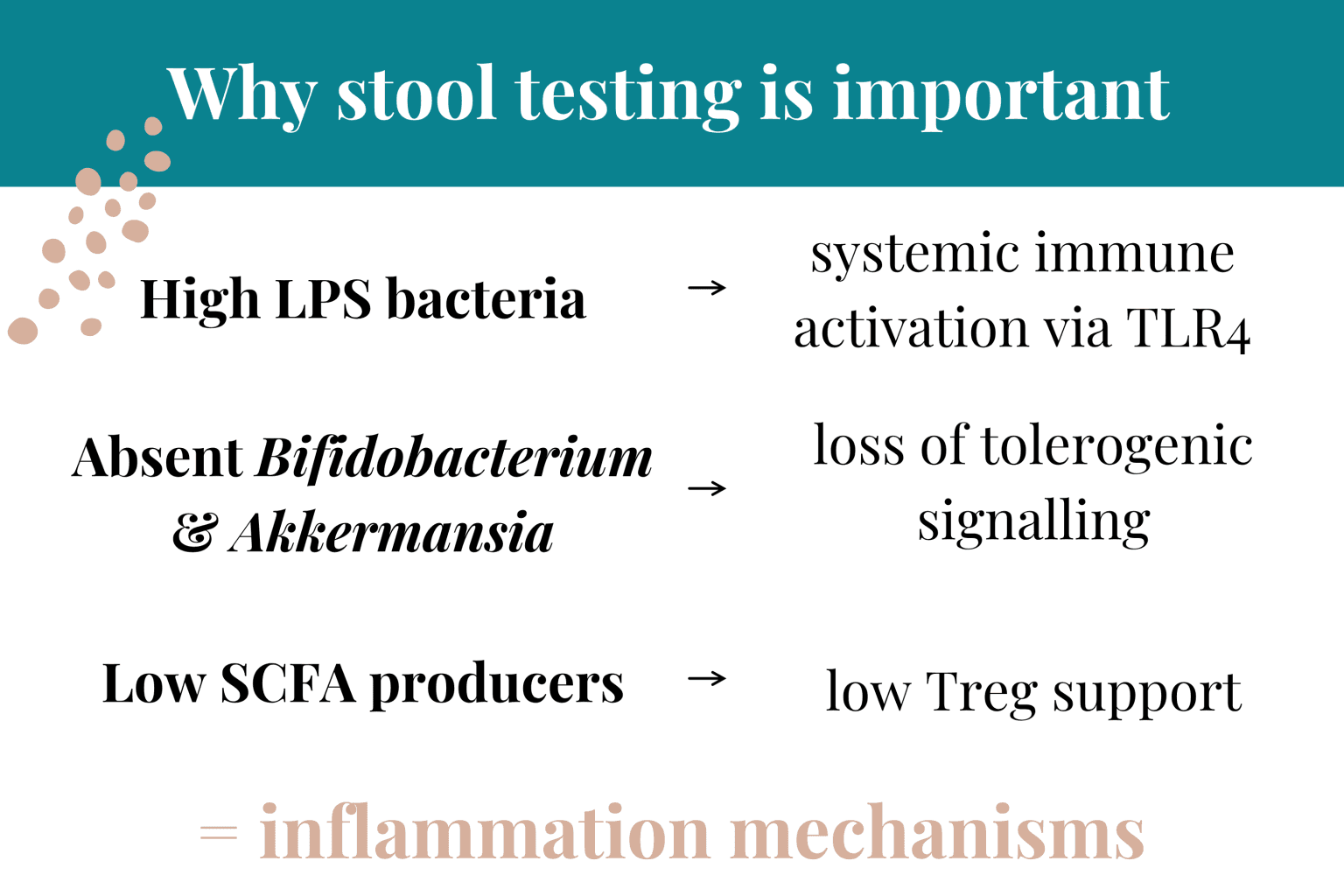
How does having enough good bacteria prevent psoriasis? F. prausnitzii, for example, plays a role in fighting inflammation via butyrate (anti-inflammatory SCFA) production.
Why Topical-Only Approaches Fail
It's natural to reach for creams, ointments, or medicated washes when your skin is flaring. In fact, for many of us, topical treatments are the first (and sometimes only) advice we're given. And while these can bring short-term relief, they rarely deliver lasting change—especially for chronic or recurring conditions.
Why?
Because skin issues driven by gut dysfunction are fundamentally immune and metabolic in nature, not just surface problems. Topical treatments may suppress inflammation or soothe symptoms on the outside, but they can't address the cascade of signals, triggers, and imbalances happening inside your body.
Here's What the Science (and Our Clinic Experience) Shows
Immunity Starts in the Gut: Over 70% of your immune system is concentrated along your gut lining, constantly training itself by interacting with gut microbes and dietary compounds. When this ecosystem is disrupted, immune cells are more likely to overreact—not just in the gut, but in distant organs like the skin.
Metabolites Matter: Beneficial gut bacteria produce short-chain fatty acids (like butyrate), tryptophan metabolites, and other anti-inflammatory molecules that help regulate skin barrier function and keep inflammation in check. When your gut isn't making enough of these, skin integrity suffers—no cream can substitute for these missing signals.
Chronic Inflammation Is Systemic: Topical steroids and immunosuppressants may dampen inflammation in one spot, but the drivers—such as microbial imbalances, food intolerances, and leaky gut—remain unchecked. The result? Flare-ups return, often with greater intensity or in new places.
That's why the best skin healing results come when you work from the inside out. Addressing the root causes—gut ecology, barrier integrity, immune balance—sets the stage for genuine, lasting improvements in skin health.
What to Do
Since gut dysbiosis is at the core of most of these skin issues, you'll want to look at the causes and treatments for gut dysbiosis.
Potential Causes of Gut Dysbiosis Include:
Overuse of antibiotics and antibacterial supplements
Too much sugar, processed foods, and food additives
Exposure to harmful chemicals and toxins from foods (e.g., pesticides)
Too much alcohol
Oral health concerns
High-stress lifestyles
Infections—parasite, bacterial, viral
Read more: What Is Gut Dysbiosis?
When Diet & Skincare Aren't Enough: Why Testing Matters
You've been doing everything right. You've eliminated gluten and dairy, you're eating fermented foods, you've switched to gentle, fragrance-free skincare products, and you're managing stress. But your skin is still flaring—eczema patches that won't heal, psoriasis plaques that keep returning, acne that persists despite clean eating.
Here's what you need to understand: Diet and lifestyle can support healthy skin, but they can't always restore a severely imbalanced gut-skin axis.
Why Diet and Skincare Aren't Always Enough
1. You Don't Know Which Anti-Inflammatory Bacteria Are Missing
Eating anti-inflammatory foods and using gentle skincare supports skin health—but only if you have the bacterial species that produce anti-inflammatory compounds.
If your Faecalibacterium prausnitzii (butyrate producer with systemic anti-inflammatory effects) is severely depleted, eating fermented foods won't rebuild this specific population quickly enough. If your Akkermansia muciniphila (strengthens gut barrier) is low, your intestinal permeability remains high—allowing inflammatory compounds to reach your skin regardless of what you eliminate from your diet.
Without testing, you're guessing which bacterial species are missing.
2. Elevated Inflammatory Bacteria May Be Driving Skin Inflammation
You might be eating perfectly and using ideal skincare, but if you have elevated Klebsiella, Proteus, or Escherichia (bacteria that produce inflammatory lipopolysaccharides), those organisms will continue triggering systemic inflammation regardless of your diet.
LPS enters the bloodstream, triggers immune responses, and manifests as skin inflammation—psoriasis, eczema, acne, rosacea. Dietary changes alone can't eliminate established bacterial overgrowths—you need targeted antimicrobials.
3. Histamine-Producing Bacteria May Be Triggering Skin Reactions
If you have chronic hives, unexplained rashes, or skin that reacts to "everything," you might have histamine intolerance driven by bacteria that produce histamine or degrade histamine poorly.
Klebsiella pneumoniae, Proteus mirabilis, and certain E. coli strains produce histamine. Eating low-histamine foods helps—but if these bacteria are elevated, they're producing histamine internally regardless of your diet. Testing identifies whether histamine-producing bacteria are the root cause.
Read more: Histamine Intolerance and Your Gut
4. Your Gut Barrier May Be Severely Compromised
If you have significant intestinal permeability (leaky gut), eating anti-inflammatory foods helps—but healing the barrier requires more than diet. You need specific nutrients (L-glutamine, zinc carnosine, butyrate), targeted probiotics (Akkermansia muciniphila, Lactobacillus plantarum), and potentially elimination of foods triggering immune responses.
Without testing, you don't know if your gut barrier is compromised or which interventions will repair it most effectively.
What Testing Reveals
When Victoria reviews comprehensive metagenomic test results for clients with chronic skin conditions, she identifies:
Depleted anti-inflammatory bacteria (Faecalibacterium prausnitzii, Akkermansia muciniphila, Bifidobacterium)
Elevated inflammatory bacteria (Klebsiella, Proteus, Escherichia, Streptococcus)
Histamine-producing or histamine-degrading bacterial imbalances
Functional capacity (Is your microbiome producing butyrate? Are inflammatory metabolites elevated?)
Gut barrier integrity markers (Are LPS levels high? Is intestinal permeability evident?)
This information allows us to create a targeted protocol:
Specific antimicrobials for inflammatory bacterial overgrowths
Targeted probiotics and prebiotics for depleted anti-inflammatory species
Gut barrier repair protocols (nutrients, specific strains)
Dietary modifications based on YOUR bacterial balance
Histamine management if histamine-producing bacteria elevated
The Bottom Line
If you've been eating clean, using gentle skincare, and managing stress for 3+ months and still have chronic skin issues—the problem isn't your effort. It's that you're working blind.
Testing shows exactly what's happening in your gut-skin axis, which bacterial species are missing, and which interventions will actually address the root bacterial imbalances driving skin inflammation.
Book Your Free Evaluation Call
Your Skin Reflects Your Gut – But Which Bacteria Are Missing?
Research shows gut bacterial imbalances drive psoriasis, eczema, acne, and rosacea. But which bacteria is YOUR gut missing?
Our AIM Method combines comprehensive metagenomic testing (reviewed by Victoria, our in-house microbiologist) with personalised protocols that target YOUR specific bacterial deficiencies and overgrowths affecting skin health.
We don't recommend generic elimination diets or skincare routines. We identify which bacterial imbalances are driving YOUR skin inflammation.
Book a free 15-minute evaluation call to discuss your skin symptoms and whether testing could reveal which gut imbalances are affecting your skin.
Book Your Free Evaluation Call
Why Personalised Gut Testing Changes Everything
You may be wondering, "How do I know if my gut is at the root of my skin issues?"
This is where the new science of microbiome and gut function testing can transform your approach.
Unlike Generic Protocols, Personalised Testing Lets Us:
Pinpoint imbalances in specific gut bacteria linked to skin inflammation (e.g., low Akkermansia or high Proteobacteria)
Measure markers of leaky gut, inflammation, and digestive enzyme function
Identify hidden infections, parasites, or yeast overgrowths that may be fuelling immune reactions
Map your individual microbial anti-inflammatory capacity and inflammatory responses
Our process combines advanced stool testing, targeted symptom assessment, and a deep dive into your health history.
This data-driven approach uncovers patterns you might never see by trial and error, and helps us design a healing plan that fits your biology—not just a textbook.
What Real Healing Looks Like: An Individual Roadmap
True gut-skin healing is never one-size-fits-all. Here's what a successful roadmap often includes:
1. Gut Barrier Repair: Gentle, low-reactivity nutrition to support healing of the intestinal lining—sometimes using functional foods and supplements like bone broth, zinc, glutamine, or marshmallow root—always check with your practitioner before considering supplements.
2. Microbiome Rebalancing: Targeted prebiotics, postbiotics, and, when lacking, specific probiotic strains (e.g., Saccharomyces boulardii, Lactobacillus rhamnosus GG), introduced gradually and monitored for individual response.
3. Immune Modulation: Identifying and removing hidden food triggers, managing stress, and supporting immune regulation using both nutritional and lifestyle strategies.
4. Lifestyle and Environment: Addressing sleep, stress, movement, and even topical routines—since what you put on your skin can also influence the gut via the skin-gut-immune axis.
5. Continuous Reassessment: Healing isn't linear. Retesting and realigning the plan based on progress and changing needs is key—what works at the start may need updating as your gut and skin recover.
Book Your Free Evaluation Call
Find Out Which Bacterial Imbalances Are Driving Your Skin Inflammation
Your chronic skin condition—psoriasis, eczema, acne, rosacea—isn't "just a skin issue." It's a signal that your gut microbiome is imbalanced, your gut barrier is compromised, or inflammatory bacteria are triggering systemic immune responses.
But eating clean and using gentle skincare products without knowing your bacterial balance is guesswork.
At Prana Thrive, we use our AIM Method to identify which bacterial species are depleted, which inflammatory bacteria are elevated, and which interventions will actually restore gut-skin balance:
Analyse — Comprehensive metagenomic testing reveals your levels of Faecalibacterium prausnitzii (anti-inflammatory), Akkermansia muciniphila (gut barrier), Bifidobacterium (immune regulation), inflammatory bacteria (Proteobacteria, Streptococcus), and histamine-producing species. Reviewed by Victoria (our in-house microbiologist) and Amanda (after analysing over 2,000 microbiome tests specialising in skin conditions).
Integrate — A personalised protocol designed for YOUR bacterial imbalances. If testing shows depleted Faecalibacterium, we focus on butyrate support and anti-inflammatory interventions. If testing shows elevated inflammatory bacteria, we use targeted antimicrobials. If histamine-producing bacteria elevated, we address histamine pathways. Not generic gut health advice—targeted protocols based on your test results and skin symptoms.
Monitor — Ongoing support with regular check-ins, protocol adjustments, and retesting to ensure your gut barrier is healing and skin inflammation is resolving. We track your progress for 3–6 months until your skin clears and gut symptoms improve.
This isn't guesswork. It's precision.
We've helped over 2,000 clients clear their chronic skin conditions by identifying which bacterial species are missing or producing inflammatory compounds—not by recommending another elimination diet or skincare routine.
Book a free 15-minute evaluation call to discuss your skin symptoms, gut health history, and whether comprehensive testing is right for you.
We work with a limited number of clients each month to ensure everyone receives personalised attention. If you're ready to stop treating symptoms and address the root bacterial imbalances driving your skin inflammation, book your call now.
Book Your Free Evaluation Call
No pressure. No obligation. Just clarity on which gut imbalances are affecting your skin.

