The Complete Guide to IBS
Plus Natural Solutions That Help
Author:
Amanda Ledwith, BHSc Naturopathy
Last Updated:
19 Jan 2026
Reading Time:
22 mins
Categories:
Gut Health
ibs
What You'll Learn
Irritable Bowel Syndrome (IBS) is a functional gut condition characterised by altered bowel habits and abdominal pain without detectable structural abnormalities. It's the most commonly diagnosed gut condition worldwide.
IBS Types (Rome IV Criteria):
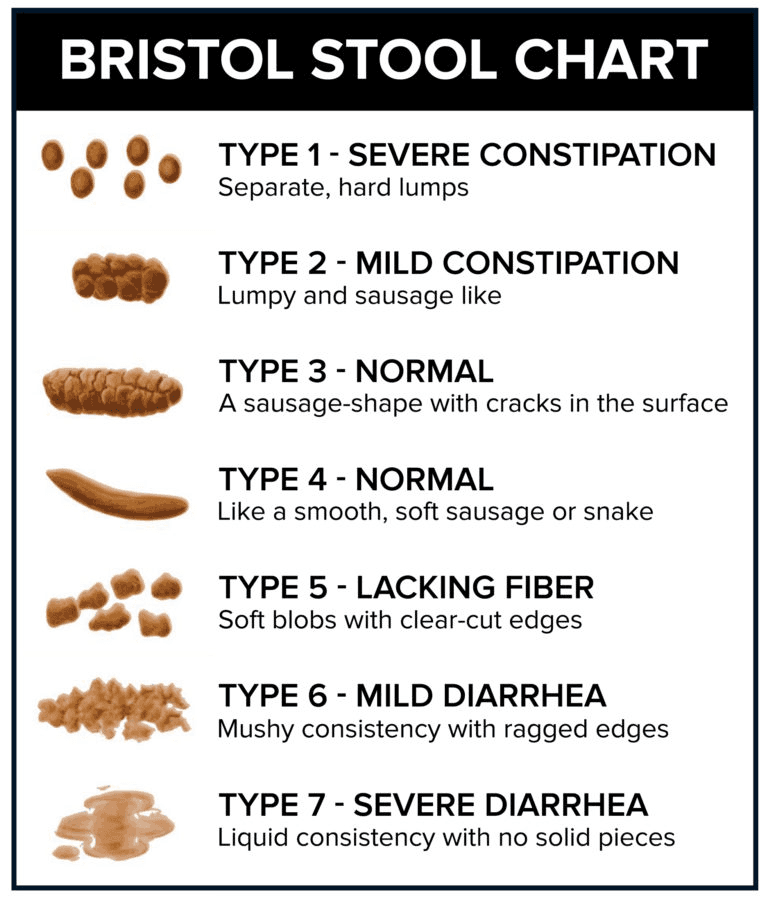
IBS-C — Predominant constipation (Bristol Stool Chart types 1-2)
IBS-D — Predominant diarrhoea (Bristol Stool Chart types 6-7)
IBS-M — Mixed/alternating constipation and diarrhoea
IBS-U — Unclassified (meets IBS criteria but doesn't fit subtypes)
Key IBS drivers:
Dysbiosis (gut microbiome imbalance)
Gut-brain axis dysfunction and serotonin dysregulation
Post-infectious changes (PI-IBS)
Chronic stress and psychological factors
Low-grade intestinal inflammation
Bacterial overgrowth (SIBO)
Why testing matters: IBS symptoms vary enormously between individuals, making generic protocols ineffective. Comprehensive microbiome testing reveals which specific bacterial imbalances, overgrowths, or missing beneficial species are driving YOUR symptoms—allowing targeted protocols rather than trial-and-error approaches.
Have you learnt to predict the outcome of your day based on your first toilet visit? Will today bring an effortless landslide or the faecal gridlock… Perhaps it will be a surprise – both!?!
Do you leave the house dreading the after-lunch gurgle and desperate loo dash – hoping to get into the quiet cubicle… and not too many visitors? Has your belly just not been right since that time you had a tummy upset?
These changes happen suddenly.
Or for some of us they progress over time, our bowel habits might even begin to take over our lives.
Either way – we should be the ones in the driver seat!
The first cases of irritable bowel syndrome (IBS) emerged over 150 years ago – it's now the most commonly diagnosed functional gut condition – worldwide!
What does this all mean?
That globally, we live amongst millions of people who dread their toilet habits.
And while this may sound silly and invite a sprinkling of harmless toilet humour – IBS has serious implications.
How Can You Measure a Healthy Gut?
IBS means business. It demands attention – pain, urgency, straining, bloating, fatigue, flatulence…
Contrast this to a healthy gut that works away quietly in the background. Only bothering us on waking – pain free, with minimal gas or bloating. Ready for whatever it gets fed.
So if all this tummy attention isn't normal…what is?
To gain a bit of perspective, it helps to know what we expect of a 'healthy' gut.
Toilet bowl clues Yup, we are going there. As much as it's not glamorous, talking about toilet habits is here to stay. You may have heard the phrase, 'what does your poo say about you?' and it's true, changes in our poop can indicate something isn't quite right.
You're looking for medium brown, soft, formed sausages that are easy to pass and not-too-smelly… If you are unsure what this all means, a great place to start is the Bristol Stool Chart. In 1997 researchers at the University of Bristol developed the chart as a medical assessment tool – and it's still relevant today.
We are aiming for chart types 3 or 4.
Ask: When did you last take a peek at your poop. Make it a habit to keep a mental note – so you get to know what your 'normal' is…Regularity of Movements How often you go, and how this changes over time is another great indicator of a healthy pooping habit. Once in the morning on waking is largely viewed as optimal.
Many people however find their normal is twice a day without any ill effects. All this is also largely dependent on the quantity and quality of food that you consume – not just underlying conditions.
Problems are indicated when the passage of passing is too short (diarrhoea) or too long (constipation).
Ask: What does my 'normal' schedule look like…?Tolerance for foods Food intolerances are becoming more and more common. Just as gut troubles are becoming more common. If you have a sudden onset of food intolerances it is a red flag that your gut isn't happy.
Being able to tolerate small quantities of many different foods is a sign of good gut health.
However, over time we may become sensitive to foods like gluten, dairy, eggs, soy etc… And it's these intolerances that signal something is amiss…
Ask: Are they any foods that I regularly avoid? Make a list.Digestion sound effects Another great indicator of a content gut is quiet digestion. Food churning, and swishing through your intestines naturally makes some noise.
Ideally at a volume that you don't feel you have to apologise for – post-eating. Hungry tummy growls are not what we are talking about here.
If you've ever been in a quiet room or post-lunch meeting where you keep hearing your gut gurgle loudly – it's a sure sign of gut distress. Maybe you've even something that you're not digesting well, or perhaps excess gas from your busy microbiome has begun to accumulate.
Either way it's uncomfortable.
Ask: How loud is my digestion normally?
These are just some of the macro- or human-sized signs we can track.
Fortunately for us, healthy base-line microbiomes have been catalogued over the years and we have a pretty good idea of what 'normal' looks like. We will talk more about this later…
Just remember that 'normal' varies for everyone…we are the microbial sum of all our experiences…our microbiome signatures are unique.
Despite this, there are trends and ranges that we can measure against.
So how is poor gut health measured…?
What is IBS?
Poor gut health can manifest as many different conditions – some serious others minor particularly when we catch them early.
Irritable Bowel Syndrome is just one of the many gut conditions that can have serious implications.
But what is it really?
IBS is clinically described as altered bowel habits in association with abdominal discomfort or pain in the absence of detectable structural abnormalities…
…what that means in everyday terms … A bowel that is irritated – at not at ease.
IBS is simply a medical term used to describe bowel habits that are different from normal without a physical cause for the discomfort and changes experienced.
Basically, the precise causes of IBS have largely evaded medical science for some time.
It's such a varied and complex cluster of symptoms that varies from person-to-person.
History of IBS
Because of this, a number of IBS sub-groups have developed over time.
But before we go through each of them, it helps to understand how these types originated.
Here's a little IBS history lesson …
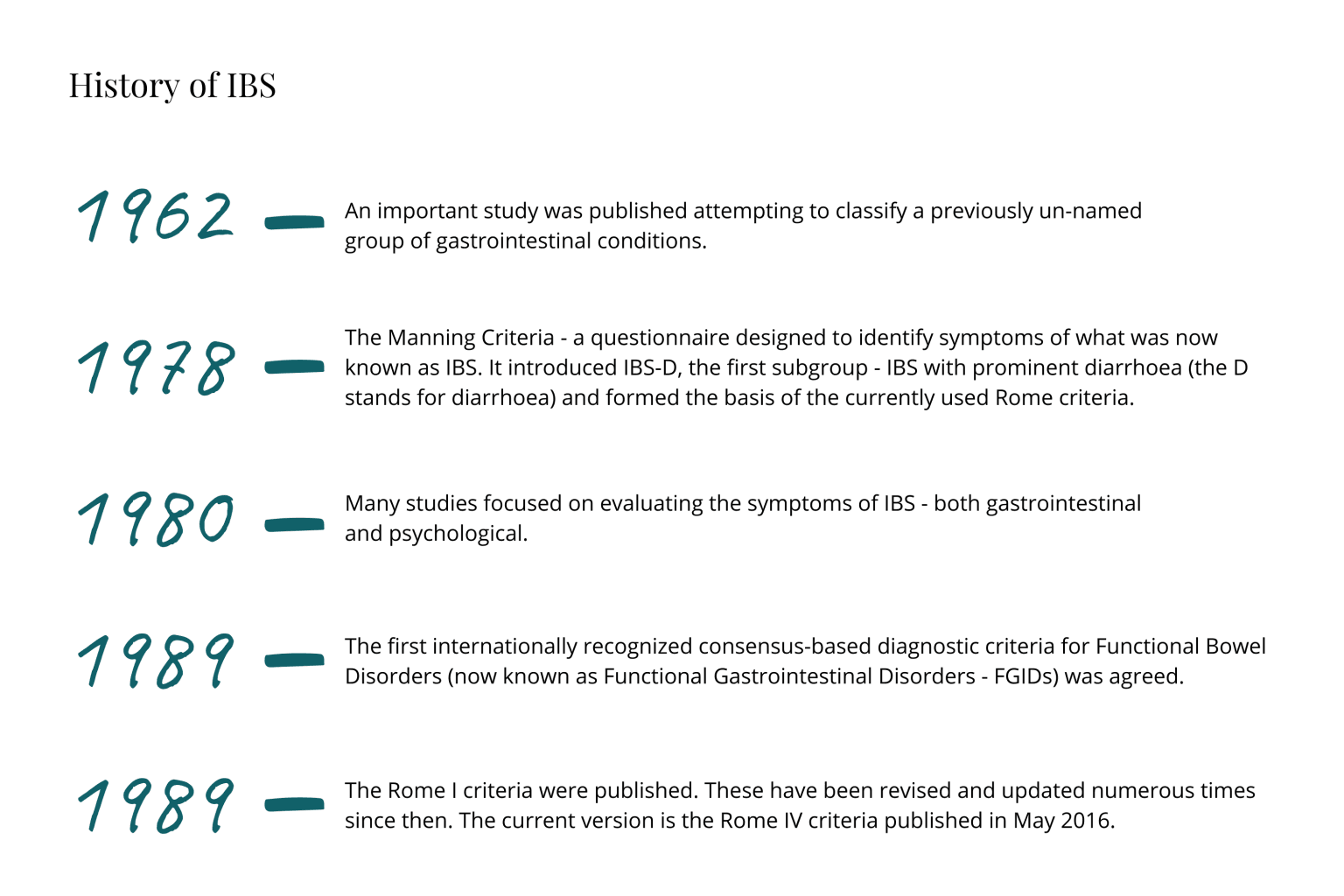
In 1962 an important study was published attempting to classify a previously un-named group of gastrointestinal conditions. The study referred to a condition they term The Irritable Colon Syndrome.
The next big development came in 1978 as the Manning Criteria – a questionnaire designed to identify symptoms of what was now known as IBS. It introduced IBS-D, the first subgroup – IBS with prominent diarrhoea (the D stands for diarrhoea) and formed the basis of the currently used Rome criteria.
Interestingly, one of the key researchers Ken W Heaton working on the Manning Criteria, also helped develop the Bristol Stool Chart we mentioned above.
From here, well into the 1980's many studies focused on evaluating the symptoms of IBS – both gastrointestinal and psychological. In 1989, the first internationally recognised consensus based diagnostic criteria for Functional Bowel Disorders (now known as Functional Gastrointestinal Disorders – FGIDs) was agreed.
It wasn't until 1994 that the Rome I criteria were published. These have been revised and updated numerous times since then. The current version is the Rome IV criteria published in May 2016.
The Rome criteria don't just include IBS but that's all we will cover here, the criteria are achieved through international consensus and set forth by the Rome Foundation based in the US.
IBS Diagnostic Criteria & Types
So what are the Rome IV criteria for IBS…?
… "Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
Related to defecation
Associated with a change in frequency of stool
Associated with a change in form (appearance) of stool …"
These criteria need to be present for the last 3 months with symptoms occurring for at least 6 months prior to diagnosis.
The types of bowel movements that are observed are then used to further categorise IBS into the following subtypes….
Type | Abbreviation | Criteria |
IBS with predominant constipation | IBS-C | Where abnormal bowel movements are usually constipation – type 1 and 2 on Bristol stool chart – for greater than 25% of abnormal bowel movements |
IBS with predominant diarrhoea | IBS-D | Where abnormal bowel movements are usually diarrhoea – type 6 and 7 on Bristol stool chart – for greater than 25% of abnormal bowel movements |
IBS with mixed bowel habits | IBS-M | Where abnormal bowel movements are usually both constipation (type 1 or 2) or diarrhoea (type 6 and 7) – for greater than 25% of abnormal bowel movements each |
IBS unclassified | IBS-U | For anyone who has bowel habits that fit into the IBS diagnostic criteria but not into any of the sub groups |
A few interesting points to note…
IBS-M was previously called IBS-A (alternating)
Rome IV is stricter than the previous versions only acknowledging pain rather than discomfort in the diagnostic criteria
Psychological symptoms are so prevalent in IBS that IBS is included in the American Psychological Association Diagnostic Manual of Mental Disorders (DSM-V)
PI-IBS (post-infectious IBS) is also common following acute gastroenteritis however it is also not well understood, acknowledged, or treated effectively
How Debilitating is IBS Really?
While the diagnostic criteria don't sound too harrowing – pain on defecation for a few months – the full complement of symptoms associated with IBS can be intense.
Ok here we go …
GI symptoms may include:
Abdominal pain
Changes to stool consistency or frequency
Constipation
Diarrhoea
Alternating constipation and diarrhoea
Straining on defecation
Urgency
Incomplete bowel emptying
Bloating and gas
Early full feeling (satiety)
Nausea
Abdominal fullness
Food intolerances
Non-GI symptoms:
Fatigue
Feelings of serious illness
Heartburn
Muscle aches
Sleep disturbances
Sexual dysfunction
Low back pain
Headache
Anxiety
Depression
Other mental health issues
Abdominal pain is the primary IBS symptom – pain that occurs below your chest but above your hips. But the term 'pain' doesn't quite do the symptom justice as many people experience varying levels of pain.
From cramping or gas-type pain… to stabbing, sharp or even migraine-like pain in their gut!
The pain is associated with how the bowel moves before, during or after a bowel movement. For some people it's constant, others frequent and is often described as excruciating, unbearable, or intense…
Another frustrating feature of IBS is that symptoms may change over time making it difficult to recognise. And easy to confuse with other gut conditions.
What's the Difference Between IBS and IBD?
Which brings us to the often asked question … how is IBS different from IBD?
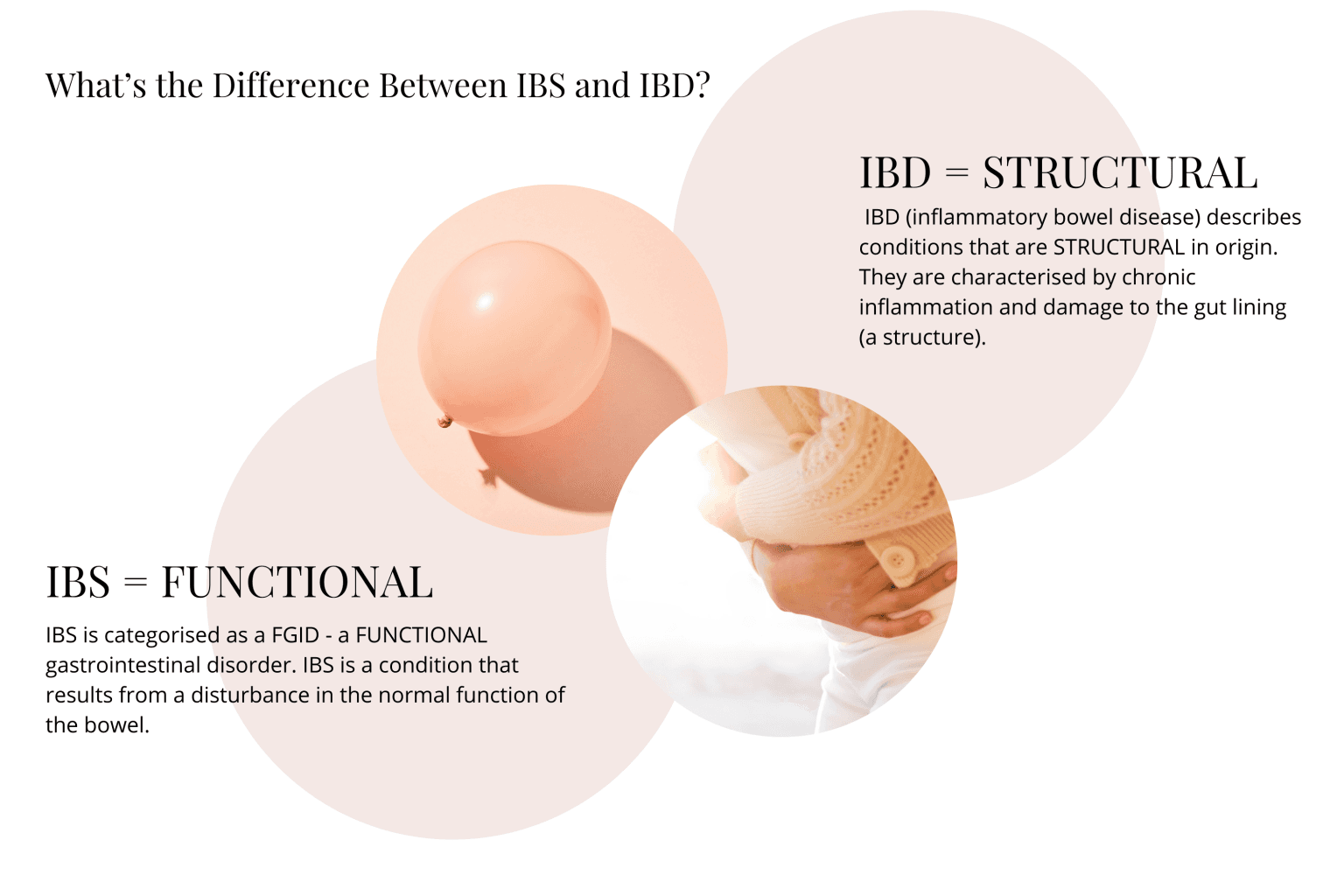
To answer this we have to remember back to our IBS history lesson – where IBS was categorised as a FGID – a FUNCTIONAL gastrointestinal disorder.
That's the clue…
… IBS is a condition that results from a disturbance in the normal function of the bowel.
Abnormal functioning of nerves and gut muscles in concert with strong gut-brain crosstalk result in the 'irritated' or highly sensitive bowel state described by IBS. Because of this crucial connection, symptoms may be triggered by emotional, stressful or even normal events.
Whereas IBD (inflammatory bowel disease) describes conditions that are STRUCTURAL in origin. In particular ulcerative colitis (UC) and Crohn's disease are the most common IBD conditions.
They are characterised by chronic inflammation and damage to the gut lining (a structure). And produce additional symptoms that are not seen in IBS.
Symptoms NOT Characteristic of IBS
Anemia
Blood in stools
Unexplained weight loss
Fever
If you experience any of those it's important to notify your doctor as these are presentations of IBD or bowel cancer in extreme cases.
By now I bet you are wondering…but what causes IBS? If it's just functional, and not structural why can't we find a therapy that works to treat it?
The Search for IBS Answers
The simple answer here is we know a little more about IBS than we used to and can treat it with conventional medicine, to a point. The symptoms can be somewhat managed, in some individuals, but largely the huge variation in symptoms varying from person to person hinders general treatment options.
So what do we know about IBS?
Physiological characteristics associated with IBS include:
Altered intestinal motility
Hyper-sensitive gut nerve networks
Gut infections causes highly reactive gut states
Changes in the gut microbiome
Bacterial overgrowth
Food sensitivities
Inability to absorb carbohydrates and sugars
Intestinal inflammation
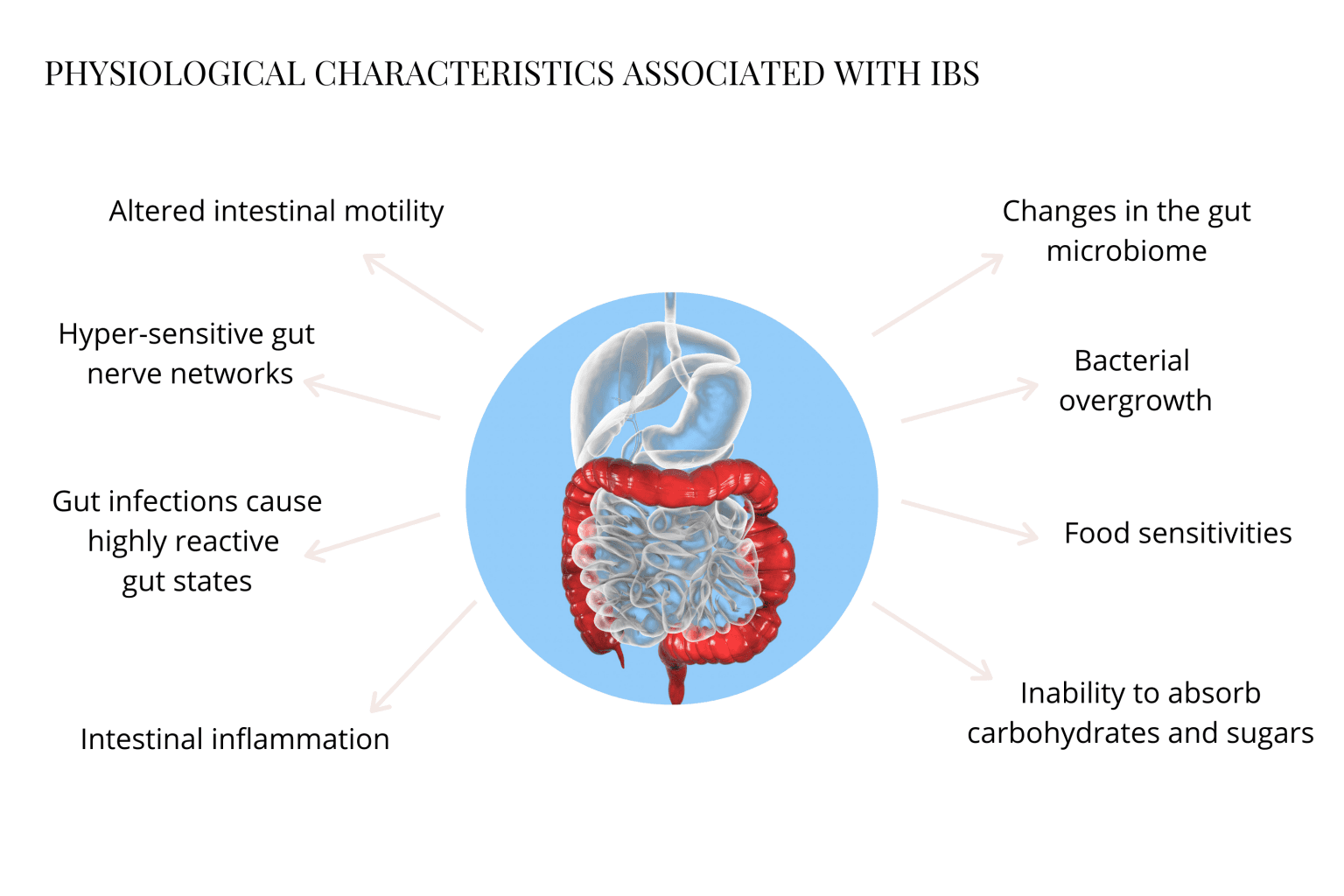
This all points to a number of potential links which have begun to be explored. We will look at a few here.
The first link we will explore hinges on the gut-brain connection.
Serotonin Dysregulation
Serotonin regulation is abnormal in IBS sufferers.
Remember that serotonin is our happy hormone and we cover it and its effects in greater detail in Gut-Brain Connection and How it Affects Your Mood. What's interesting in IBS is researchers have identified two abnormalities in how serotonin is regulated.
Serotonin release into plasma is lower with IBS-C and higher in IBS-D sufferers
A serotonin signalling defect has been detected in both IBS and UC – transporter molecules in the gut lining are reduced.
These findings are an important step towards acknowledging the psychological effects of gut conditions.
But they also point to a 'what came first?' scenario as IBS has now been proven to have conclusive psychosocial links.
For example, those with a history of abuse are significantly associated with IBS but this doesn't necessarily predict IBS prevalence – there are many other factors involved.
But what it does indicate (and there is substantial evidence for) is stress and IBS are very closely associated.
Stress
Stress plays a pivotal role in the development of IBS. So much so that IBS has been described as a combination of irritable bowel AND irritable brain.
Mounting evidence suggests that psychological stress not only contributes to IBS development but exacerbates symptoms. Some of these stress-IBS impacts include:
Intestinal sensitivity
Motility
Secretion
Gut lining permeability
Mucosal immune activation
Altering of the Central Nervous System (CNS)
Peripheral nerves
Microbiome
All from stress!
IBS is described as a stress-sensitive disorder indicating that treatment absolutely must include effective stress-management for success.
Many of our IBS clients indicate they work in high-stress professions or have had significant emotional stressors in their lives.
Lack of sleep is another big stressor in IBS – but more on that later.
Various types of stress changes on neuroendocrine-immune pathways act on the gut-brain axis and the microbiota-gut-brain axis resulting in flare-ups and further immune activation.
Infection and Immune Activation
Activation of the immune system and inflammation are nearly synonymous. Without inflammation our bodies would be ill-equipped to tackle day-to-day life and the various threats we constantly face.
Here we are going to focus on infection induce immune activation and the connection with IBS. If you are interested in learning more about our important Gut-Immune System Connection you can read our extensive article on the topic.
Many clients struggling with IBS symptoms can recall an infectious event that started their IBS journey. This is what we referred to above as PI-IBS, post-infectious IBS.
Where viral tummy-bugs run their course and seem to have limited and short-term effects, bacterial and parasitic infections are risk-factors for developing IBS.
Infections like:
Salmonella
Shigella
Campylobacter
Traveller's diarrhoea
Clostridium difficile
Blastocystis
Cryptosporidium
Giardia
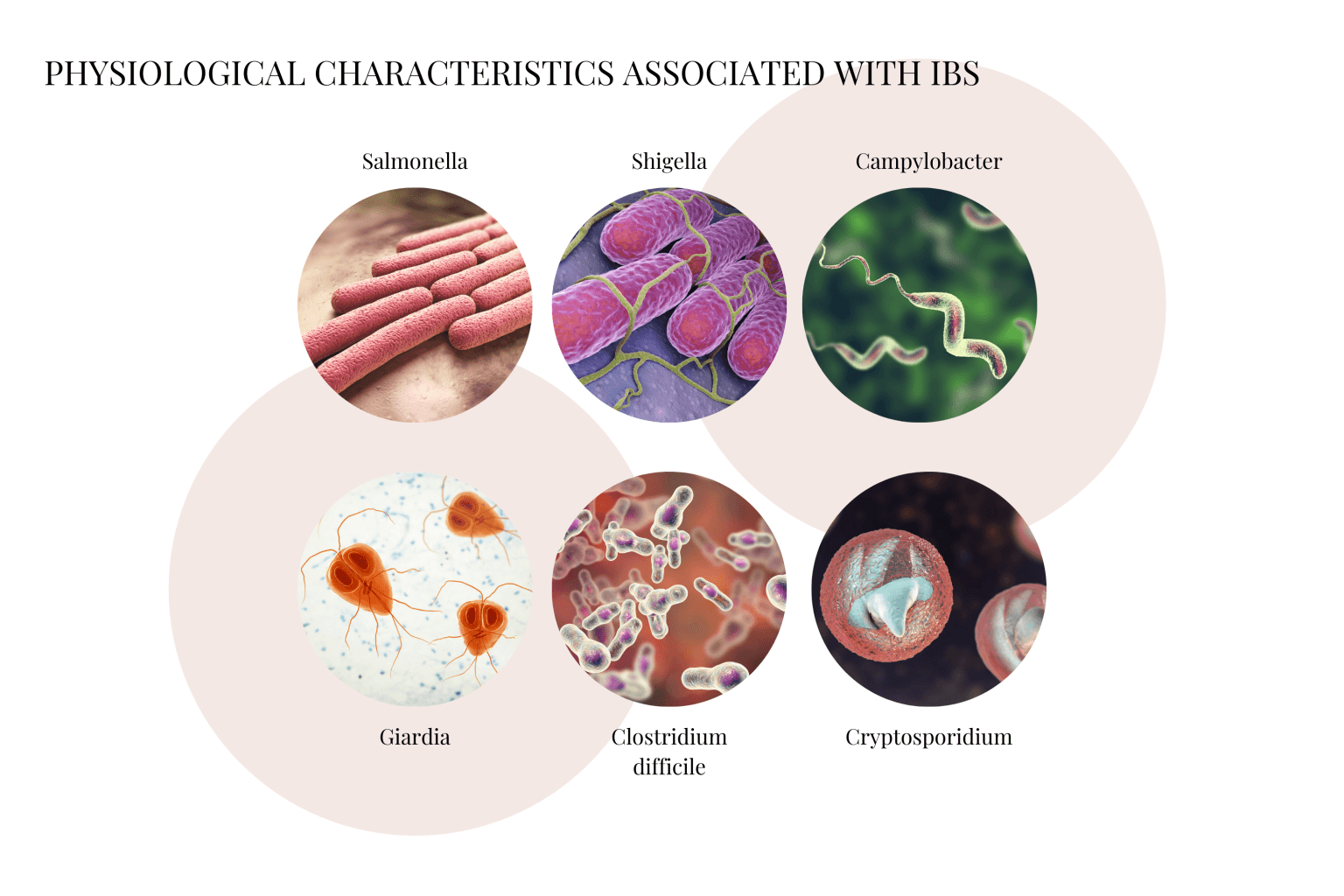
Further risk factors for PI-IBS development include, having a prolonged initial illness, smoking, inflammation markers, depression, recent adverse life events and of course the toxicity of the infective strain.
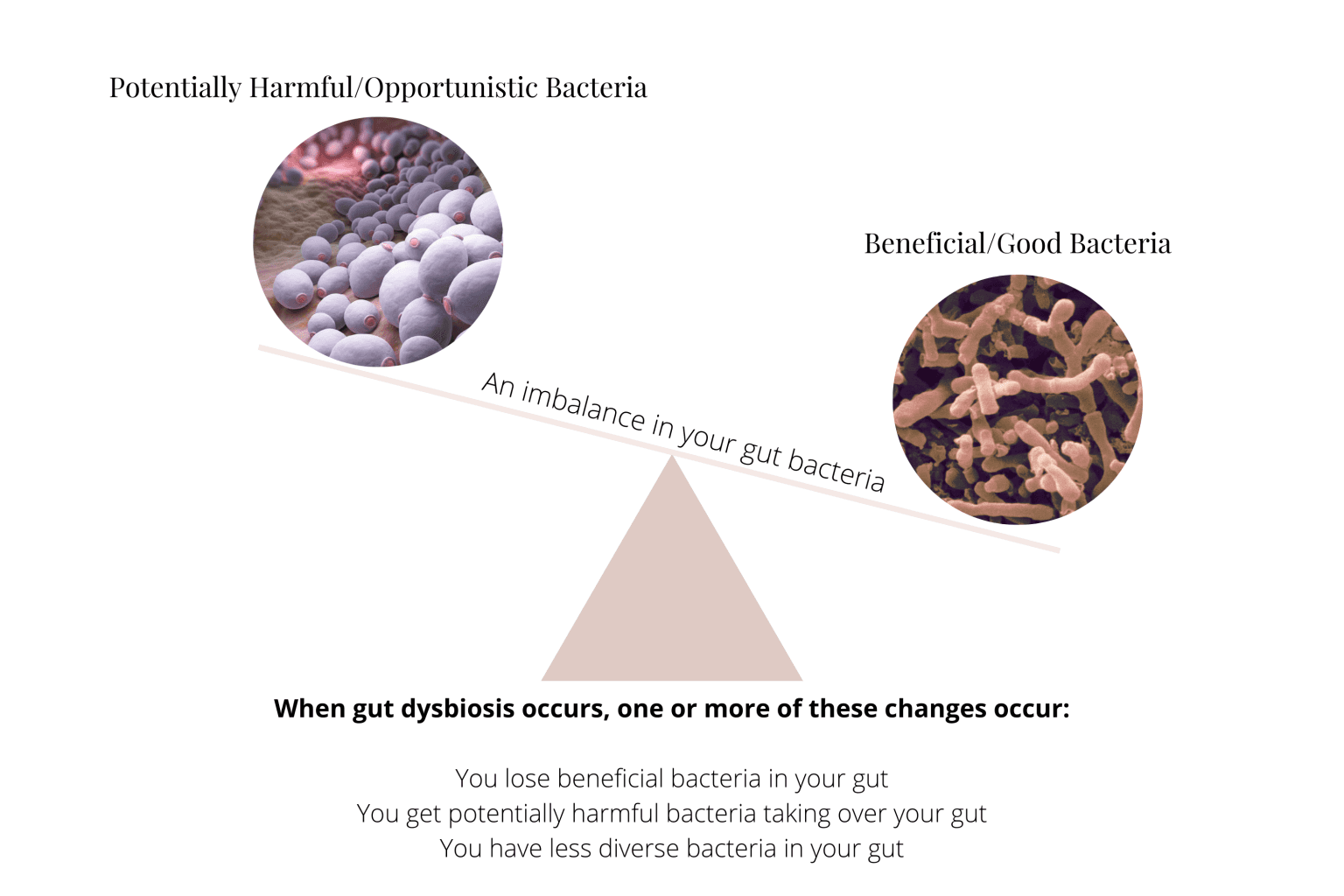
These infectious organisms, or pathogens, tend to shift the balance of the gut microbiome. Their presence is largely self-serving and ultimately induces a state of imbalance where beneficial bacteria find it hard to survive.
And so begins an important IBS predictor and the cascade into microbial tyranny – dysbiosis.
The Microbiome and IBS
Your gut is a complex ecosystem housing a dense and diverse microbial community. We co-evolved with our bacterial inhabitants to play the role of host and have developed a strong mutualistic relationship.
A healthy relationship where we both benefit.
They are offered a regular supply of food and cosy intestinal shelter. And in return we receive their innumerable by-products including beneficial vitamins, nutrients and metabolites.
Altruistic give and take.
Trouble comes however, when this fragile equilibrium is lost.
Our beneficial bacteria population may decrease and no longer produce adequate metabolites that we need for our wellbeing.
Or a keystone species like Ruminococcus or Akkermansia is wiped out that guards the health of our gut lining resulting in leaky gut. Perhaps we change our diet and unknowingly begin to feed species that don't support our health.
This complex ecosystem collapse is called dysbiosis.
And it's a powerful predictor of IBS.
So much so, that with every gut microbiome test we request for our clients, we include a specific IBS test. Because the microbiome changes that accompany IBS are diverse and complex.
IBS Microbiome Trends
The nuances of the IBS gut microbiome is too much to cover here, but in general, an overall decrease in beneficial species like Lactobacillus and Bifidobacterium is seen. In severe cases these important probiotic species can be completely absent!
And this probiotic-absent profile is very often accompanied by increases in non-beneficial bacteria and pathogens. Like Streptococcus, Klebsiella, Citrobacter, some enterococci species and many in addition to those mentioned above.
And just like the huge diversity in IBS symptoms and type-profiling, there is no one-size fits all for IBS gut microbiome profiling either. Making it absolutely crucial that you find an experienced health professional to work with who has extensive experience with gut microbiome testing and interpretation.
If you are looking to get to the bottom of your IBS symptoms and address them at the cause we offer comprehensive gut testing packages.
All our offerings are expertly tailored to your individual results and health history we also consider other concerns or conditions you may have in a holistic way.
Because in many cases IBS doesn't exist in isolation. It has many other conditions connected with it. Particularly gut-brain associated illnesses.
🔬 VICTORIA'S EXPERT INSIGHT
"When I review microbiome test results for clients with IBS, I'm looking for specific patterns that explain why conventional treatments often fail—and what targeted interventions will actually work.
What I assess in IBS cases:
1. Dysbiosis patterns specific to IBS subtype IBS-C, IBS-D, and IBS-M each have distinct microbiome signatures. In IBS-C clients, I consistently see reduced Bifidobacterium species and low short-chain fatty acid (SCFA) production—which explains the slow motility. In IBS-D, I often find elevated Klebsiella, Citrobacter, or Enterobacter species driving inflammation and rapid transit. IBS-M clients typically show the most complex dysbiosis patterns, often with both bacterial overgrowth AND depleted beneficial species.
2. SIBO markers Many IBS diagnoses are actually undiagnosed SIBO (small intestinal bacterial overgrowth). When I see elevated hydrogen-producing bacteria (Klebsiella, certain Streptococcus species) alongside symptoms of bloating within 30-60 minutes of eating, I know SIBO testing and targeted antimicrobials are likely needed—not just generic IBS protocols.
3. Missing keystone species In nearly every IBS case, I find critically depleted keystone species—bacteria that perform essential functions for gut health. Akkermansia muciniphila (gut barrier protection), Faecalibacterium prausnitzii (anti-inflammatory), and Roseburia species (butyrate production) are commonly absent or severely reduced. Rebuilding these species is essential for long-term resolution.
4. Post-infectious patterns (PI-IBS) For clients whose IBS started after food poisoning or traveller's diarrhoea, I look for residual pathogenic organisms (Blastocystis, Dientamoeba, Campylobacter) and the dysbiosis they've caused. These cases require addressing the initial infection before microbiome restoration can succeed.
5. Histamine-producing bacteria Many IBS clients also have histamine intolerance symptoms (headaches, skin flushing, anxiety alongside gut symptoms). I check for elevated histamine-producing bacteria (Morganella, certain Lactobacillus species, Klebsiella) which can drive both gut and systemic symptoms.
The critical insight: There is no single 'IBS microbiome'—each person's bacterial imbalances are unique. This is why generic IBS diets and probiotics often fail. Testing reveals YOUR specific dysbiosis pattern, allowing targeted protocols that address root causes rather than just managing symptoms."
— Victoria, Microbiologist
Book Your Free Evaluation Call
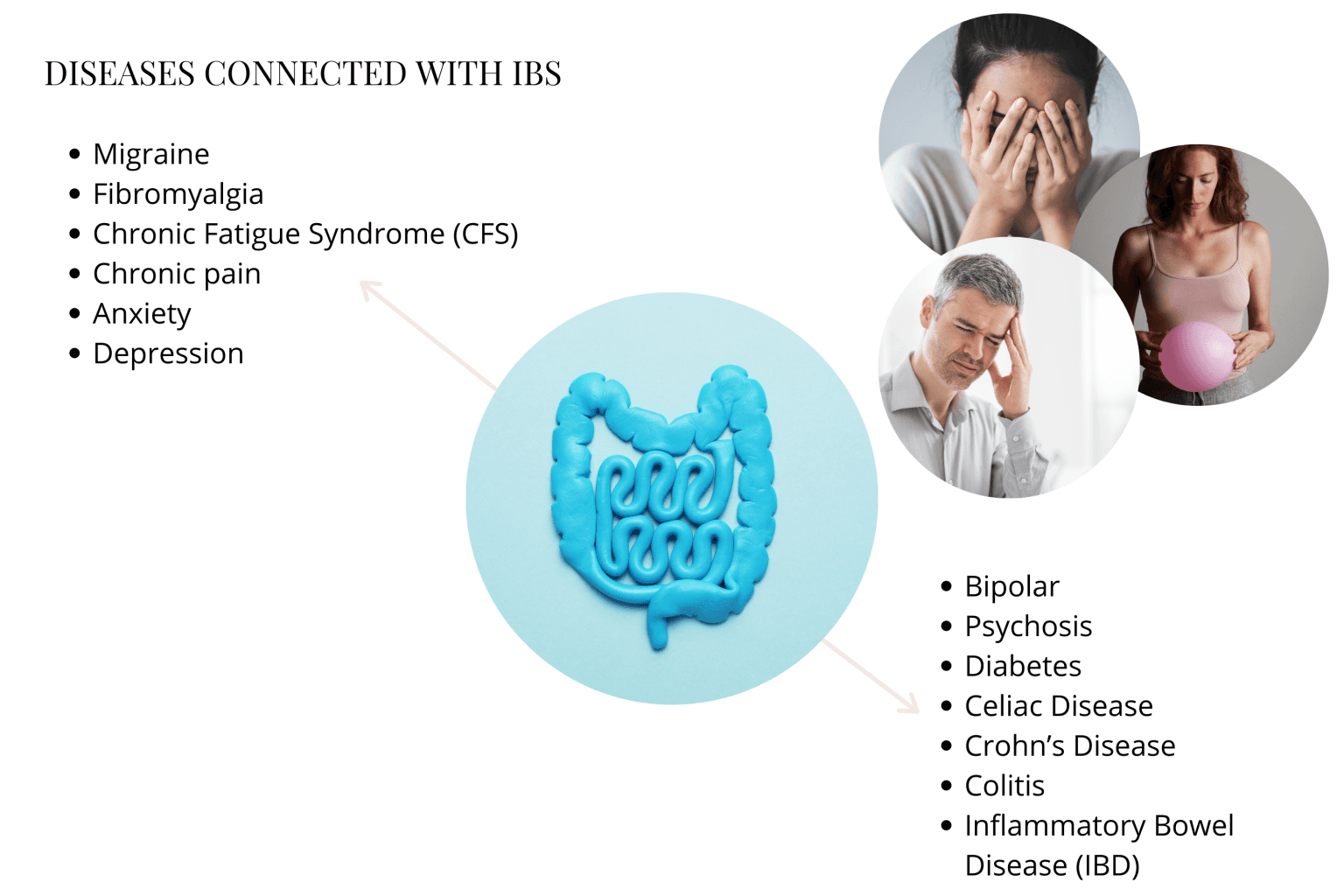
Diseases Connected with IBS
Diseases that often present in combination with each other are termed comorbidities. And the most prevalent comorbidities seen with IBS are psychological and psychiatric conditions.
As we have seen depression and anxiety go hand-in-hand with IBS. And largely mood disorders and anxiety are the most common presentations to show up with IBS. But they are not the only conditions to the partner with IBS.
Other diseases connected with IBS include:
Migraine
Fibromyalgia
Chronic Fatigue Syndrome (CFS)
Chronic pain
Anxiety
Depression
Bipolar
Psychosis
Diabetes
Celiac Disease
Crohn's Disease
Colitis
Inflammatory Bowel Disease (IBD)
And when you look closely, there is something that many of these conditions have in common…
… inflammation.
Whether it be in the gut, or in the brain – or both – inflammation is a constant companion for those suffering with IBS.
Inflammation Starting in the Gut
More and more, emerging evidence is demonstrating how inflammation may play a huge and detrimental role in IBS.
At the microscopic level in IBS, inflammation in the gut lining is persistent over time and in many causes begins to overlap with chronic inflammatory bowel disease (IBD).
In particular, IBS gut hypersensitivity may be positively correlated with increased mast cell density and activity.
Mast cells are a type of white blood cell that play an important role in inflammation in response to infection, insect, venom or allergy triggers. They typically cause 'allergic' symptoms and promote inflammation.
This mechanism is evidenced by those suffering from post-infectious IBS where an initial event triggers systemic inflammation, alters the gut microbiome and creates a low-level chronic inflammation response.
Additionally, neuro-inflammation or brain inflammation via the gut-brain axis is also an active pathway in IBS. Ultimately giving rise to an overall pro-inflammatory state and dysregulated serotonin functioning which in part may account for many IBS symptoms.
And while research into anti-inflammatory treatments continues at full steam – the conventional treatment of IBS remains difficult due to its layers of complexity and diversity.
Which begs the question, if there are already many effective natural treatment options for inflammatory conditions, could these be of benefit in IBS?
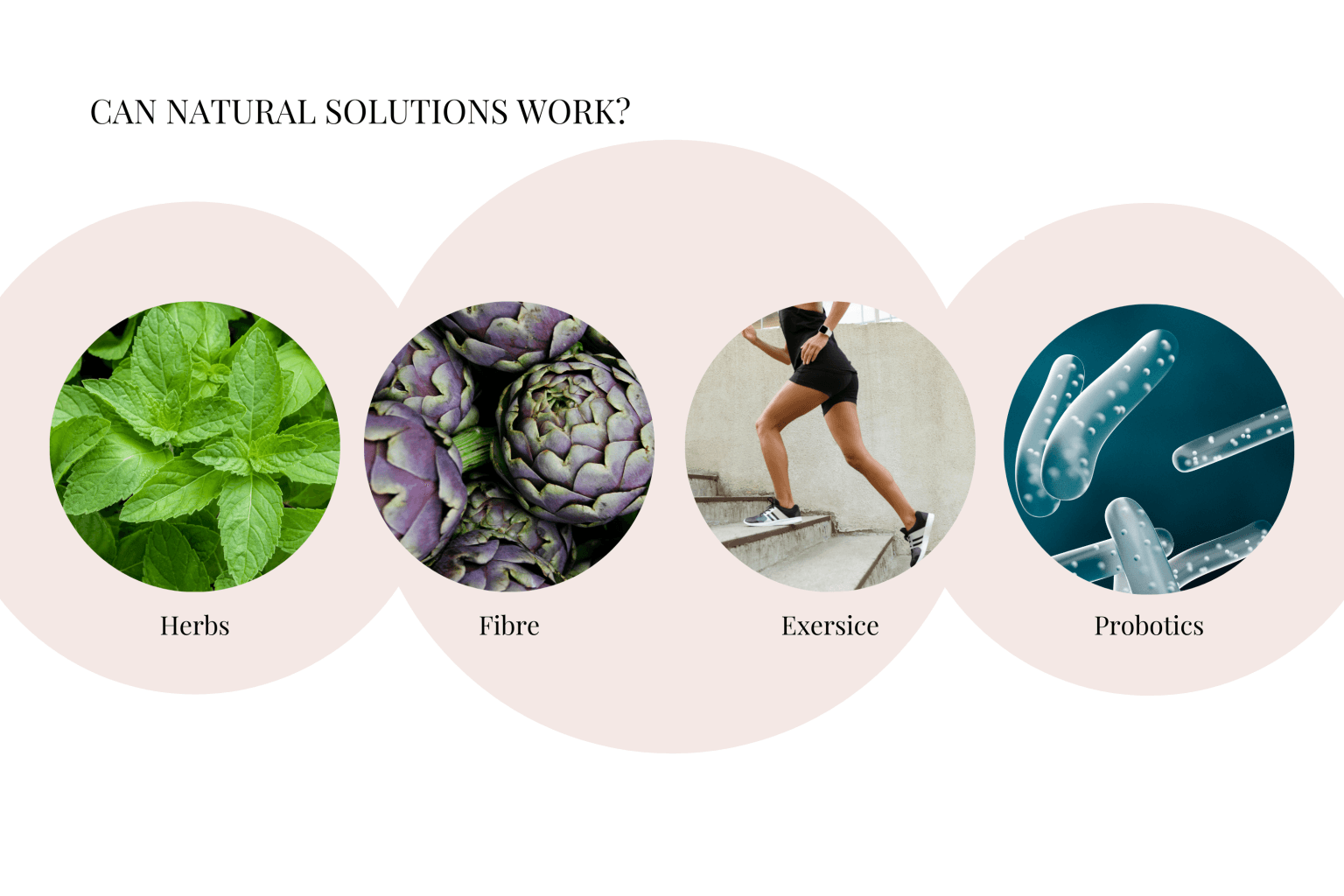
Can Natural Solutions Work?
Preliminary evidence is promising. And to be clear, by natural solutions, we mean any intervention that is not of chemical origin.
Let's take a look at a few common natural remedies now.
Herbs Aloe, peppermint oil, turmeric and others have been shown to be effective in the management of various IBS symptoms. Aloe shows promise in IBS-C with constipation relief, peppermint oil via it's antispasmodic properties and turmeric for its famous anti-inflammatory action.
Herbal solutions are generally well tolerated and don't tend to come with the many side effects common with pharmaceuticals. As always it's important to work with a qualified natural health professional to determine what is right for your individual circumstancesFibre Artichoke, psyllium and fibre obtained from fruits and vegetables has been shown to reduce bloating symptoms. The addition of a bulking fibre like psyllium husk to those suffering with IBS-C can alleviate constipation symptoms.
In general, an increased consumption of soluble fibre (prebiotics) has been shown to benefit IBS symptoms in general, including constipation.Exercise A common natural remedy prescription, exercise in various forms helps to improve IBS symptoms. This includes (but is not limited to):
Bicycling for less symptom aggravation and gas relief Yoga twice daily may be as effective as conventional loperamide treatment Breathwork (or traditional yogic pranayama) helps to increase gut muscle tone
Additionally, in a study focused on women with IBS, physical activity was correlated with reduced fatigue.
Exercise has been proven to exhibit long-term positive effects in the treatment of both IBS gut and psychological symptoms.Probiotics Probiotic therapy for IBS is one of the most common natural treatments used. Popular preparations for IBS include Lactobacillus and Bifidobacterium species.
In particular Bifidobacterium infantis has shown significant improvement in global IBS symptoms across a number of studies. This is thought to be due to its ability to down regulate the proinflammatory state seen with IBS.
The probiotic yeast Saccharomyces boulardii has also shown promise as a preventative and a therapy.
And while there are many types of probiotics that may assist like all microbial therapies, to gain the most benefit from them it's important to know your personal levels. You can then supplement effectively for the best results – our gut microbiome testing includes testing for probiotic bacteria.
In addition to these approaches, general diet modification can reduce symptoms while working toward working on the root cause.
By removing triggers you allow the body to reduce it's inflammatory response and begin to repair the damage.
Next we will look more closely at some of the common IBS triggers to avoid.
Common IBS Triggers
Alright, now we are at the exciting part. Removing some of these common triggers, although simple, can be highly effective at reducing symptoms and getting some IBS relief.
So let's get right into it.
In no particular order, the most common IBS triggers that our clients find effective are:
The inflaming 5 foods Gluten, dairy, grains, sugar and bad oils. All these foods are proinflammatory. And as we have seen inflammation and IBS are deeply connected.
These foods work via various mechanisms which we won't go into here. If you want to know more we cover them extensively in our upcoming online program – Gut Heal & Nourish.
By removing or limiting these you are working with your body to turn down inflammation and promote healing.Repeat courses of antibiotics Taking various antibiotics over a long period of time is a known IBS trigger. Antibiotics by their designed action are anti-biotic or anti-life – they wipe out your gut microbiome. And have been likened to a bomb going off in your gut.
The microbes, viruses or fungi (including yeasts like Candida) that remain then have free rein over food supply and can run rampant. Potentially resulting in dysbiosis or further infectious states.
Taking antibiotics in childhood and particularly in youth is also a predictor of IBS.
Limiting antibiotic use unless absolutely necessary may help in reestablishing balance and preventing flare-ups.Work, emotional and trauma based stress This one is so big we are going to mention it all over again. Stress is such a huge trigger for IBS!
Working to eliminate or at least reduce stress triggers in your life is so important.
Mindfulness practices like meditation, gentle exercise, yoga and breathwork are but a few of the simple yet powerful stress busting modalities widely available around the world.
And they have science to back them up!
The next step in beginning your journey to heal with IBS is to consider lifestyle factors that may be hindering your healing.
Lifestyle Factors to Consider
Another big topic (that we talk about comprehensively in our Gut Heal & Nourish Program) are everyday lifestyle habits that promote gut health.
To get you started we will cover three of the most important (after stress reduction) here:
You are what you (and your microbes) eat Eating a wholefood, nutrient-dense, plant-predominant diet full of natural prebiotics, gut-healing resistant starch and all important minerals is absolutely key.
If you have known issues with FODMAPs – you can read more about how to get started here.
The role of food in the treatment and prevention of IBS cannot be overstated. It's just so important. Removing processed, refined and manipulated foods and food-like substances from your life is always a good idea but is vital in healing IBS.
As part of our signature Gut Microbiome Testing Program we offer an 8 week meal plan designed to help you do just that.
Additionally we have a jam-packed archive stocked with delicious gut-friendly recipes.Get enough sleep Sleep difficulties are common in those suffering with IBS. And a source of stress in itself. Sleep is also often the culprit behind day-time lethargy and fatigue, but may be difficult to achieve when dealing with chronic pain.
Maintaining good sleep practices may help:
Meditate or have a dedicated rest period before going to bed Avoid focusing on the time by not having a clock in view Maintain a routine wake-up time in spite of interrupted sleep Not staying in bed awake for more than 20 minutes – get up again until you feel sleepy Avoid stimulating beverages, foods and activities in the late afternoon and evening Use the bed for sleeping not watching TV, reading or eating Avoid daytime napping Avoid blue-light sources like your mobile phone and laptop which impair your melatonin cycles crucial for sleep
And if the problem persists ask your natural health practitioner for natural sleep aids.
Reduce your toxic load Our modern lives are full of insidious toxic substances that can have a detrimental effect on your gut microbiome. Toxins are quite literally everywhere – in our food, water, air, personal care products, clothing, beds, cleaning cupboard and more. Being mindful of these sources is the first step in reducing how much you allow into yours and your family's lives. Sourcing organic, natural alternatives to cleaners and personal care products is a great place to start. Filtering your water is another important one. Tackling your lifestyle one room at a time with the goal to reduce your exposure is not only absolutely satisfying it can also help you to heal in the long term.

