Psychobiotics
How Beneficial Bacteria Can Reduce Stress and Improve Mood
Author:
Amanda Ledwith, BHSc Naturopathy
Last Updated:
16 Dec 2025
Reading Time:
XX min
Categories:
Probiotics & Bacteria
psychobiotics
What You'll Learn
Psychobiotics are beneficial bacteria (probiotics) or support for beneficial bacteria (prebiotics) that specifically influence the gut-brain axis—reducing stress, improving mood, and supporting cognitive function.
Research shows specific psychobiotic strains can help with:
Stress response — Lowering cortisol levels and anxiety
Mood disorders — Reducing depression symptoms and aggressive thoughts
Cognitive function — Improving memory and reducing brain fog
Sleep quality — Supporting serotonin production for better rest
Key psychobiotic species include:
Bifidobacterium longum 1714 (stress, anxiety, memory)
Lactobacillus helveticus + B. longum (mood, cortisol reduction)
Lactobacillus rhamnosus (HPA axis regulation, nerve excitability)
Faecalibacterium prausnitzii (anti-inflammatory, linked to improved anxiety)
But here's what most people don't realise: Taking psychobiotic supplements without knowing your bacterial balance means you're guessing. Some people are depleted in Bifidobacterium and will benefit from B. longum. Others have adequate Bifidobacterium but are missing Faecalibacterium or other species. Testing shows which psychobiotic strains YOUR gut actually needs.
Introduction
Are you feeling confused about the latest gut health trending buzzword "psychobiotics"?
Wondering where the word came from or what psychobiotics actually are? [Hint: it's nothing to do with scary movies, full-moon antics, or otherwise crazy behaviour.]
Maybe you'd like to know the difference between a regular probiotic and a psychobiotic—or even a prebiotic for that matter.
With the fast-tracked advances in microbiome research happening globally, it can be hard to keep up with all the new terminology (and the epic discoveries).
So here I'd like to talk you through the basics of psychobiotic science, clear up the confusion, and empower you with the knowledge to face the probiotic shelf with confidence.
More importantly, I'll show you how to know which psychobiotic strains YOU actually need—because taking random supplements hoping they'll reduce stress or improve mood is expensive guesswork.
After analysing over 2,000 microbiome tests, I can tell you: some people desperately need Bifidobacterium longum for anxiety. Others have adequate Bifidobacterium but are severely depleted in Faecalibacterium prausnitzii—a key anti-inflammatory species linked to improved mood. Without testing, you won't know which applies to you.
Let's start with the basics: what psychobiotics are and how they work.
What Are Psychobiotics?
Psychobiotics are defined as "beneficial bacteria (probiotics) or support for beneficial bacteria (prebiotics) that influence bacteria-brain relationships."
To understand this statement better, let's look at the definitions of both probiotics and prebiotics:
Probiotics: Live microorganisms that offer a health benefit (specific bacteria)
Prebiotics: A substance that is selectively used by microorganisms offering a health benefit (specific food for probiotic bacteria)
In a nutshell, you can think of psychobiotics as both probiotics (specific bacteria) AND prebiotics (specific food for probiotic bacteria) that offer a health advantage specifically to the brain and nervous system.
If you've been following us for a while, you'll know that the gut is like your second brain—and it's intimately linked with your actual brain through the gut-brain axis.
How Psychobiotics Work
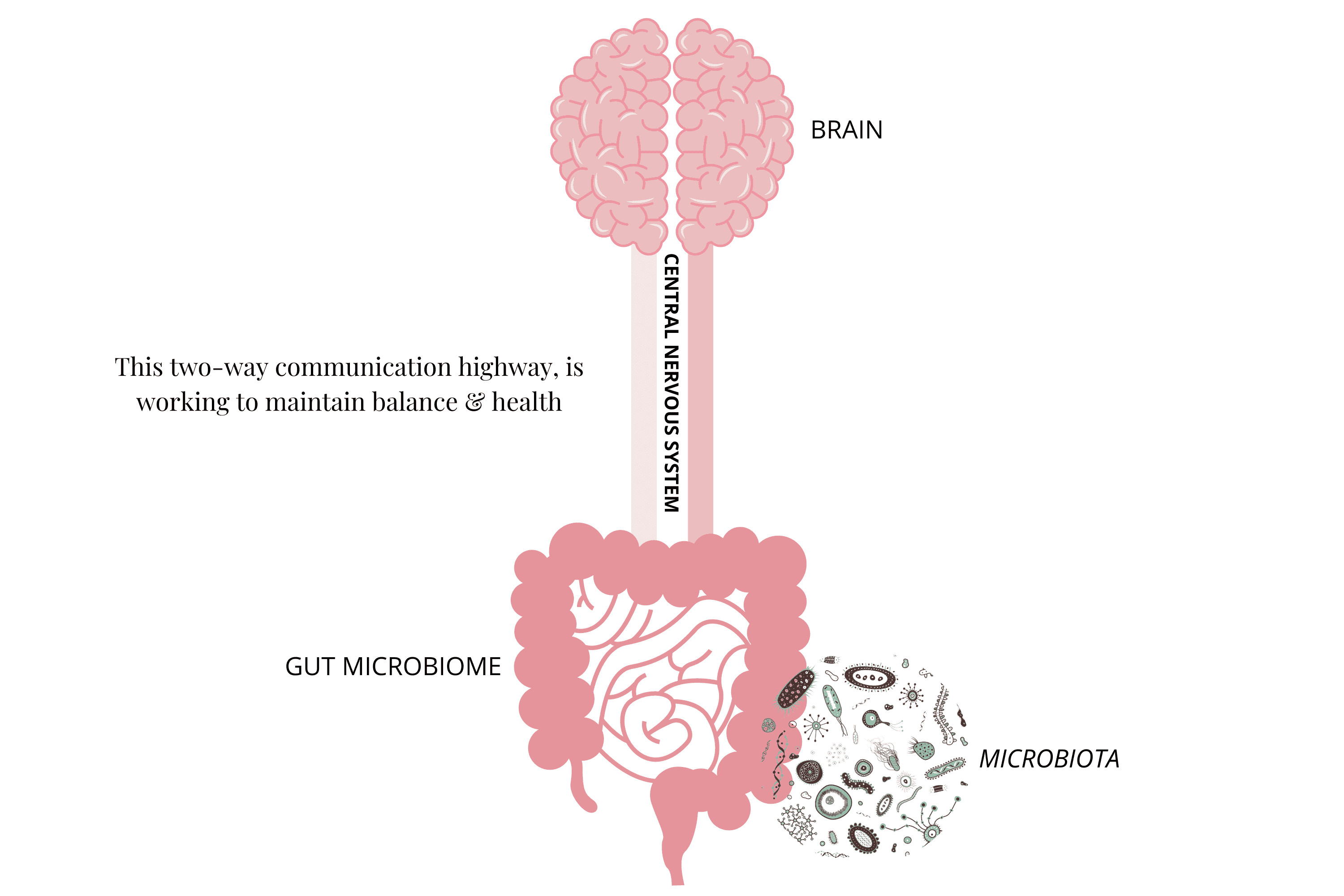
This connection is commonly known as the gut-brain axis. We'll just go over the basics here, as I talk about the gut-brain axis at length in our article "Gut-Brain Connection and How It Affects Your Mood".
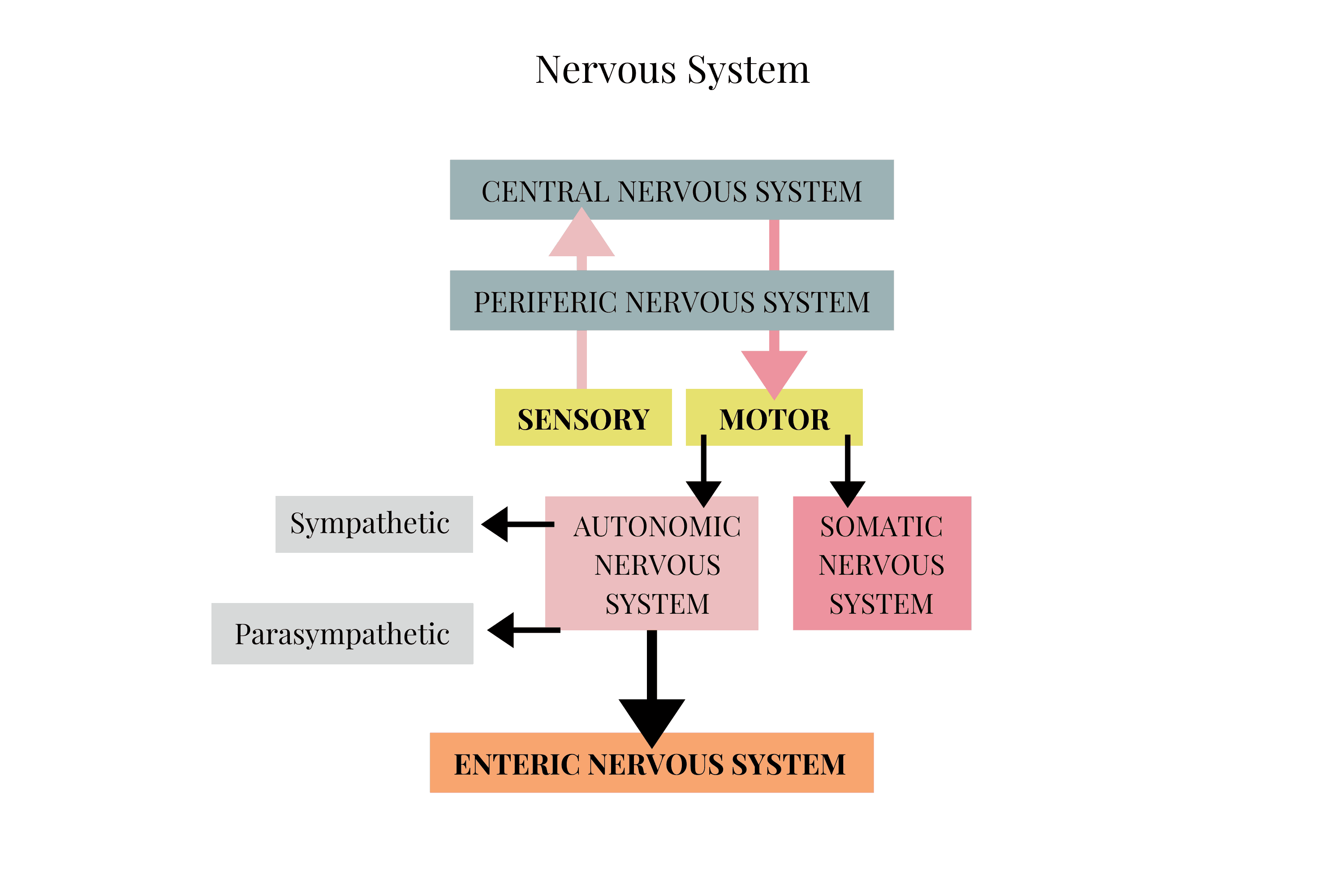
Fundamentally, your gut-brain axis includes your:
Central Nervous System (CNS) — Your brain, spinal cord, and nerves
Endocrine System — Hormones that affect the brain and nerves
Immune System — Immune functions affecting the brain
Sympathetic and Parasympathetic Nervous Systems (from Autonomic Nervous System – ANS) — "Fight or flight" and "rest and digest" respectively
Enteric Nervous System (ENS) — Your gut brain
Gut Microbiome — The bacterial ecosystem in your intestines
The general mechanism is that gut microbial by-products (like short-chain fatty acids and neurotransmitters), immune cells, and hormones can enter the bloodstream from the gut and ultimately reach the brain via the vagus nerve.
And vice versa—it's a (complex) two-way street.
Psychobiotic Mechanisms
Psychobiotics are thought to work on various gut-brain signalling pathways:
1. Bacteria-Nervous System Signalling
Bifidobacterium longum and Lactobacillus rhamnosus have been shown to influence the excitability of gut nerve cells.
2. Vagus Nerve Connection
Studies show that psychobiotic effects are transported via the vagus nerve to the brain. This nerve is the primary communication highway between your gut and brain.
3. Short-Chain Fatty Acids (SCFAs) & Bacterial By-products
Prebiotics increase production of SCFAs, which influence secretion of important satiety (feeling full) hormones that act on the brain. SCFAs like butyrate also have direct anti-inflammatory effects on brain tissue.
4. Bacteria-Immune Interactions
Reductions in pro-inflammatory cytokines have been reported due to prebiotics. Similarly, B. infantis and L. rhamnosus GG can increase anti-inflammatory cytokines, reducing systemic inflammation that affects mood and cognition.
5. Stress Hormones & the Gut Lining
Bifidobacterium and Lactobacillus species have helped restore gut lining integrity in animal studies. A stronger gut barrier reduces lipopolysaccharide (LPS) leakage into the bloodstream—LPS triggers inflammation that contributes to anxiety and depression.
Ultimately, these mechanisms affect your cognition (your ability to think clearly), learning, mood, emotions, and stress response.
Simply put, psychobiotics affect your psychological processes.
Now that we've introduced the ways psychobiotics work on the gut-brain axis, let's have a closer look at how your body registers and responds specifically to stress triggers.
How Your Body Responds to Stress
Stress affects everyone differently. Different people respond to stress in different ways.
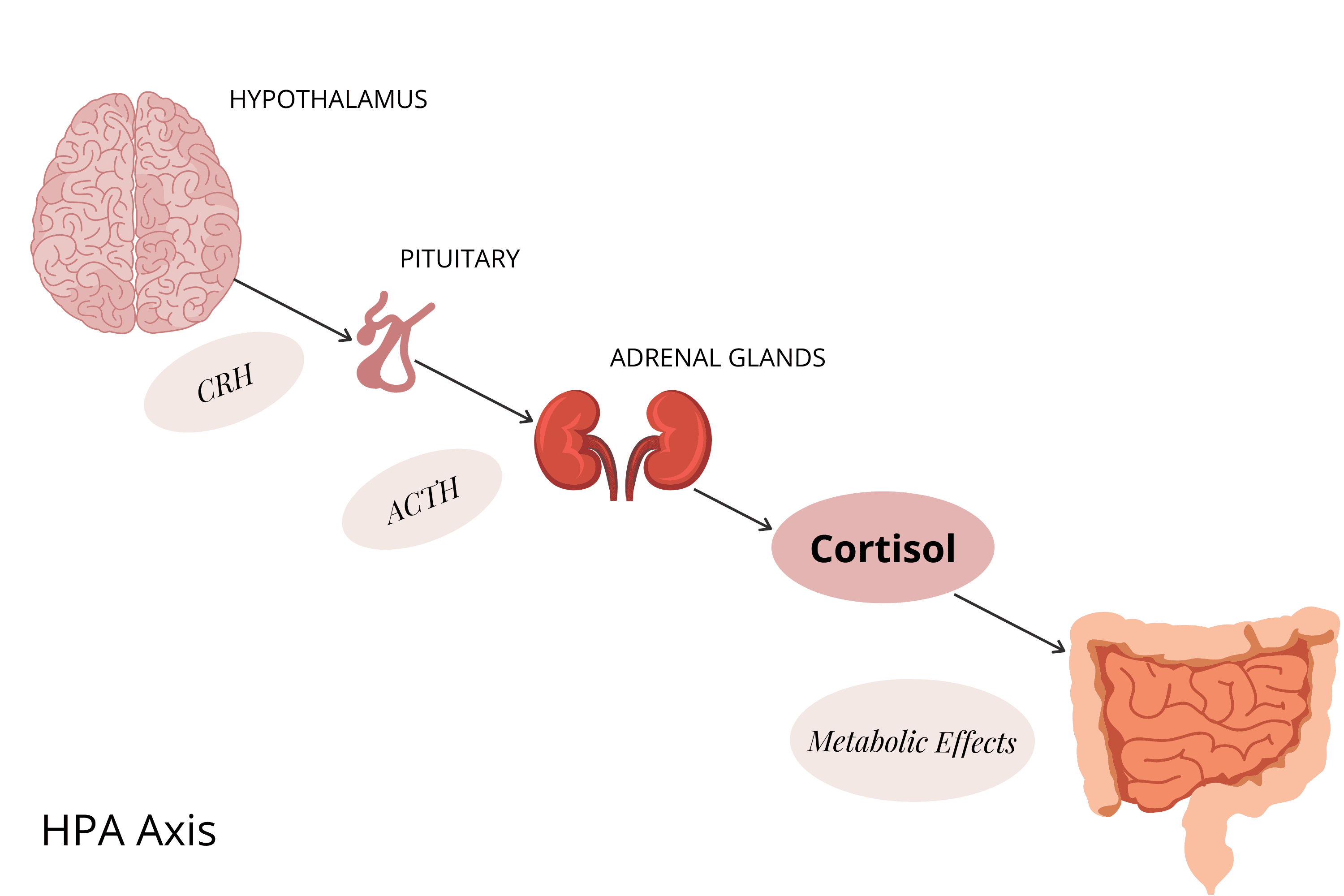
But one thing we all have in common is the pathway that mediates our stress response: the HPA axis.
Your HPA (Hypothalamic-Pituitary-Adrenal) axis is your primary pathway for stress response. Your Sympathetic Nervous System (SNS)—our "fight or flight" nerve network—works together with your HPA to determine how you react to stress.
The Stress Response Cascade
To illustrate this connection, their coordinated response to a stress trigger looks like this:
Stress hormones (adrenalin, etc.) are released into your bloodstream and tissues—by your SNS
At the same time, CRF (corticotropin releasing factor) emerges from your brain—via your hypothalamus
CRF stimulates the release of ACTH (adrenocorticotropic hormone)—from your pituitary gland
ACTH travels through your blood and triggers the synthesis (and release) of cortisol—by your adrenal glands
So it goes: stress hormones → hypothalamus (CRF) → pituitary (ACTH) → adrenals (cortisol).
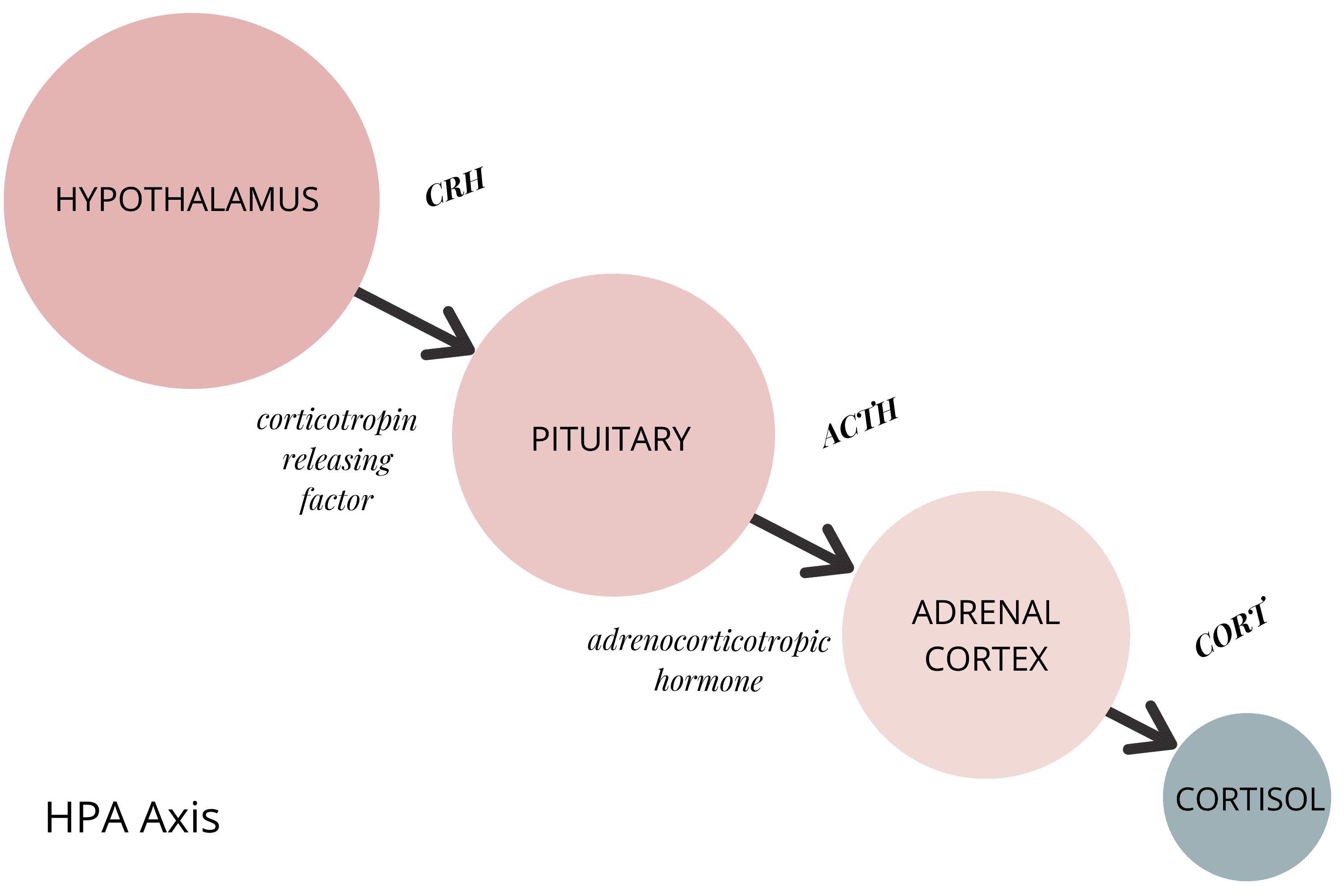
I simply want to show you the pathway stress takes—there are many more steps, but these are the basics.
The purpose of this stress response cascade is to increase blood glucose levels, suppress the immune system, and increase metabolism of fats and proteins. It's your body getting you ready for an incoming threat—preparing to "fight" or "fly" (run away fast).
The Antidote
In order to calm this response, neurotransmitters like serotonin, noradrenaline, and endorphins are needed—as well as removing the physical or psychological stress triggers, of course.
So what does all this have to do with psychobiotics?
Everything.
While we can't always remove modern-day stressors, we can definitely influence the gut bacteria that produce calming hormones.
Bacteria That Produce Stress-Busting Neurotransmitters
Serotonin Producers:
Common gut bacteria produce the stress-busting neurotransmitter serotonin. Streptococcus, Enterococcus, and E. coli have all been shown to make serotonin as part of their normal metabolism.
We can supplement or encourage these helpful species.
Did you know: 90% of our serotonin (a master calming hormone) is stored by specialised cells in our gut called ECCs (enterochromaffin cells).
GABA Producers:
Well-known probiotics like Lactobacillus and Bifidobacteria have been shown to produce stress-busting hormones like GABA (gamma-aminobutyric acid) and others. These are all psychologically supportive species—as well as being helpful in many other ways too.
Tryptophan Production:
Another important probiotic bacteria, Lactobacillus reuteri, has been associated with production of the serotonin precursor tryptophan. Tryptophan is an essential amino acid (meaning humans don't produce it).
In general, our gut microbes are thought to contribute to tryptophan availability from the food we eat. More tryptophan means more serotonin = less stress!
Prebiotics:
Prebiotics have also been shown to have beneficial stress response effects—because they directly feed the bacteria that have these beneficial effects. This is why prebiotics are included in the definition of a "psychobiotic."
How Are Psychobiotics Different From Probiotics?
By now you might be wondering: what's the difference between a regular probiotic and a psychobiotic?
The answer: their researched effect.
Psychobiotics are probiotics or prebiotics that are found to act on the gut-brain axis.
To clarify, historically probiotic research focused mostly on gastrointestinal issues. Which is why so much more is known about how gut infections and gut-specific conditions like IBS respond to probiotic treatment. There's purely been more research on these topics.
For example, it's well known that infectious diarrhoeal illnesses respond well to specific probiotics like L. rhamnosus, Saccharomyces boulardii, Lactobacillus casei, Bifidobacterium lactis, Streptococcus thermophilus—and many others.
The aim of psychobiotic research is to conduct studies on specific probiotics and find whether they significantly improve psychological outcomes. It's an exciting and brand-new field of microbiome science.
But the reality is that many (perhaps most) probiotic bacteria would be classified as both a psychobiotic and a probiotic.
For instance, L. rhamnosus (effective in diarrhoeal infections) is also linked with calming the HPA response to stress in animal studies AND also linked with affecting nerve excitability.
So it crosses both definitions. I suspect many probiotics will have the same (exciting) fate.
Which Conditions Can Benefit From Psychobiotics?
While research is still in the early stages, psychobiotic effects are beginning to emerge for some well-studied probiotic bacterial species and some prebiotics too.
A handful of the human studies conducted to date are outlined in the table below—I've already mentioned some of the animal studies above.
Condition | Psychobiotic | Action |
Bipolar | Faecalibacterium<br>L. rhamnosus GG + B. animalis lactis | Higher levels associated with improved anxiety, depression, and sleep<br>Supplementation reduced hospital visits in patients with mania |
Stress | B. longum 1714<br>L. casei Shirota<br>L. gasseri | Supplementation lowered cortisol levels, anxiety, and stress. Memory improvements were also noted<br>Lower academic stress and cortisol levels, higher serotonin post-examination<br>Athletic fatigue reduction, elevated mood post-exercise |
Mood | L. helveticus + B. longum<br>B. bifidum, B. lactis, L. acidophilus, L. brevis, L. casei, L. salivarius + L. lactis | Reduced stress (cortisol) and improved mood<br>Reduced rumination and aggressive thoughts |
Anxiety + Depression (with IBS) | B. infantis | Reduction in pro-inflammatory markers |
Negative emotions | GOS (prebiotic) | Anti-depressant effects |
As you can see, there have definitely been some positive connections made, but there is still much research that needs to be done.
Important note: These are population-level studies showing general trends. Individual responses vary dramatically based on YOUR bacterial balance. Some people respond powerfully to B. longum 1714 because they're depleted in Bifidobacterium. Others have adequate Bifidobacterium but are missing Faecalibacterium or other species—and won't benefit from B. longum supplementation.
Testing shows which psychobiotic species you're actually depleted in, so you can target the right strains instead of guessing.
Book Your Free Evaluation Call
Understanding Which Psychobiotics YOU Need
The research on psychobiotics is compelling—specific bacterial strains can reduce stress, improve mood, and support cognitive function.
But here's what the research doesn't tell you: which strains YOUR gut is missing.
Some people are severely depleted in Bifidobacterium longum and will benefit enormously from B. longum 1714 supplementation. Others have adequate Bifidobacterium but are missing Faecalibacterium prausnitzii—a key butyrate-producing species with powerful anti-anxiety effects.
Our AIM Method uses comprehensive testing to identify which psychobiotic species are depleted, which inflammatory bacteria are elevated, and which interventions will actually work for YOUR gut-brain axis.
Book Your Free Evaluation Call
Should YOU Take Psychobiotics? When Testing Matters
The research on psychobiotics is exciting—B. longum 1714 reduces cortisol and anxiety. L. helveticus + B. longum improves mood. Faecalibacterium correlates with reduced anxiety and better sleep.
But here's what I've seen after analysing over 2,000 microbiome tests: some people desperately need specific psychobiotic strains, while others have adequate levels and need completely different bacterial species.
Taking psychobiotic supplements without testing is expensive guesswork. You might get lucky—or you might waste months taking the wrong strain while your stress and anxiety continue.
When Psychobiotic Supplementation Is Likely to Help
1. Depleted Bifidobacterium Species
If your test shows low Bifidobacterium longum, B. infantis, or other Bifidobacterium species, psychobiotic supplements containing these strains (like B. longum 1714) can help regulate your HPA axis, reduce cortisol, and improve stress resilience.
2. Low Lactobacillus Species
If Lactobacillus species (particularly L. helveticus, L. rhamnosus, or L. casei) are depleted, targeted supplementation can support GABA production, nerve excitability regulation, and mood improvement.
3. Depleted Faecalibacterium prausnitzii
If your F. prausnitzii is low (common with anxiety, depression, and inflammatory conditions), supporting this species with specific prebiotics and butyrate supplementation can have powerful anti-anxiety effects—even though it's not traditionally marketed as a "psychobiotic."
4. Elevated Inflammatory Bacteria
If Victoria's analysis reveals elevated inflammatory species like Klebsiella, Proteus, or Enterobacter, these bacteria produce lipopolysaccharides (LPS) that trigger neuroinflammation. Addressing these overgrowths while rebuilding psychobiotic species creates better outcomes.
5. Post-Antibiotic or High-Stress Periods
If you've recently completed antibiotics or been through prolonged stress (which depletes beneficial bacteria), targeted psychobiotic supplementation can help rebuild protective species.
When Psychobiotic Supplementation Probably Won't Help
1. You Already Have Adequate Psychobiotic Bacteria
If your Bifidobacterium and Lactobacillus levels are normal, taking more psychobiotic supplements won't provide additional benefit. You need to identify which OTHER bacterial species are depleted.
2. Your Mood Issues Are Driven by Other Bacterial Imbalances
If F. prausnitzii (butyrate producer) or Akkermansia muciniphila (barrier integrity) are severely depleted, your anxiety might be driven by low butyrate or increased intestinal permeability—not lack of psychobiotic species. You need different interventions.
3. Fungal or Parasitic Overgrowths Are Present
If Candida overgrowth or parasites are driving systemic inflammation (which affects mood), psychobiotic bacteria won't address the root cause. You need antifungals or antiparasitics first, then rebuild with targeted probiotics.
4. You Have Active Bacterial Overgrowth (SIBO)
If you have small intestinal bacterial overgrowth, adding more bacteria (even beneficial psychobiotic strains) can worsen symptoms. Address the overgrowth first, then rebuild strategically.
Why Testing Changes Everything
When Victoria reviews your metagenomic test results, she identifies:
Current levels of psychobiotic species (Bifidobacterium, Lactobacillus, etc.)
Levels of Faecalibacterium prausnitzii and other butyrate producers
Elevated inflammatory bacteria producing stress-triggering compounds
Fungal or parasitic overgrowths affecting mood
Your gut's functional capacity (neurotransmitter production, inflammation markers)
This information allows me to recommend psychobiotics strategically—not based on marketing claims or general research, but based on YOUR specific bacterial imbalances.
The bottom line: Psychobiotic supplements are powerful when used correctly. But "correctly" means knowing whether YOUR gut actually needs them—and which specific strains.
How Can We Harness Psychobiotics to Manage Stress?
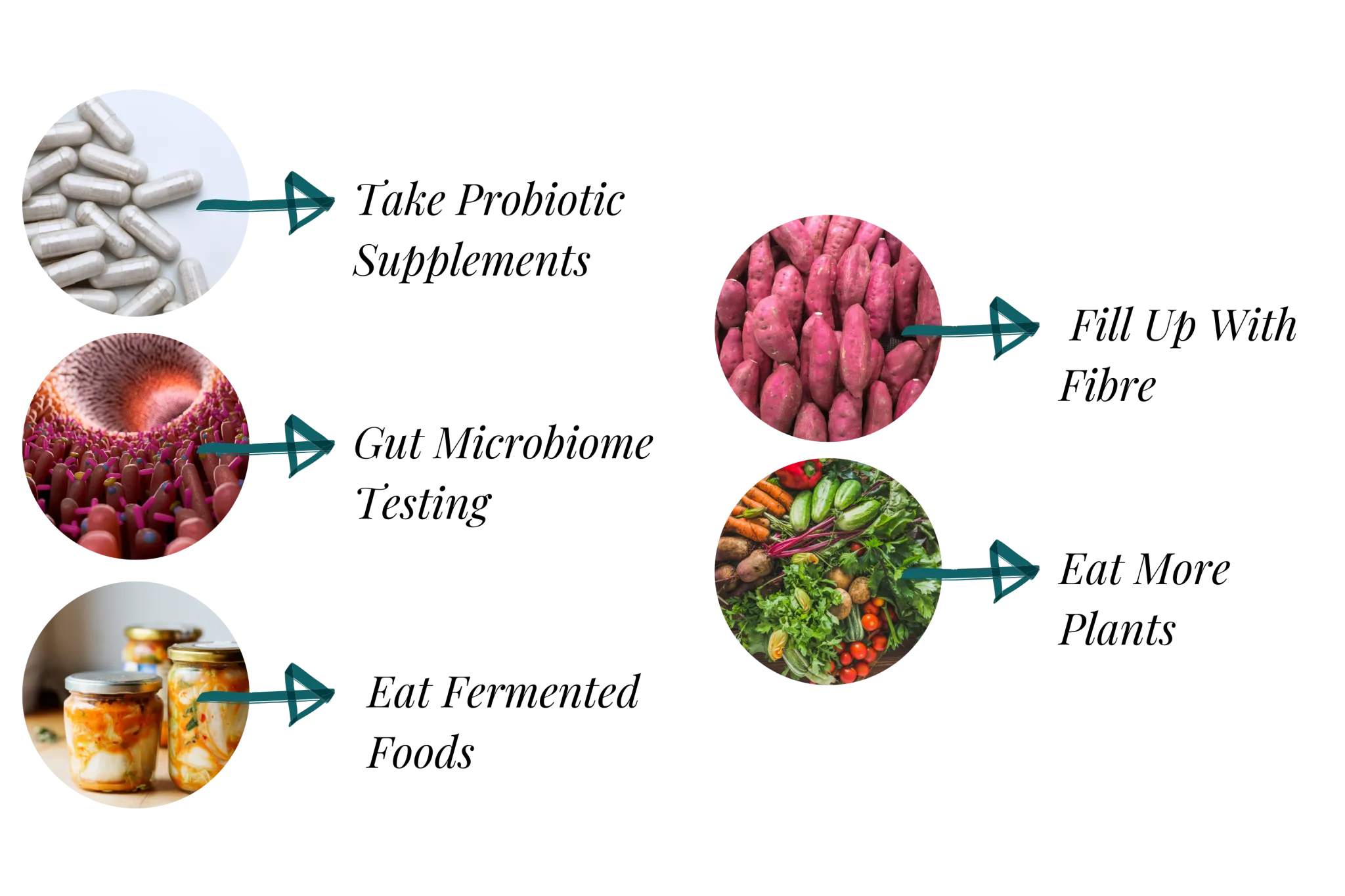
There are several ways you can tap into the positive effects of psychobiotics:
1. Comprehensive Gut Microbiome Testing
Knowing exactly which psychobiotic species you're lacking—or which inflammatory bacteria you have in abundance—is the most powerful tool for enhancing mental health. Testing identifies which specific interventions will work for YOUR bacterial balance, not generic recommendations.
2. Targeted Probiotic Supplements
High-quality practitioner-grade probiotics containing specific psychobiotic strains can support you during times of stress—when chosen based on your actual bacterial deficiencies. My clients take probiotics selected specifically based on their metagenomic test results.
3. Eat Fermented Foods
Naturally fermented foods like kimchi, sauerkraut, fermented vegetables, and fermented sauces are all great food-based sources of probiotic (and psychobiotic) bacteria.
4. Fill Up With Fibre
With brain-boosting SCFA production in mind, eating more fibre or resistant starch is always a good idea. Fibre feeds psychobiotic bacteria like Bifidobacterium and butyrate-producing species like Faecalibacterium.
5. Eat More Plants
Vegetables and fruits naturally contain many different prebiotic fibres all packaged conveniently together. They make for an easy prebiotic and fibre boost whilst supporting health and mood improvements in general too.
6. Include Stress-Busting Lifestyle Habits
Don't forget exercise, meditation, and regular sleep patterns—these support your gut-brain axis from the other direction, creating a positive feedback loop.
Book Your Free Evaluation Call
Stop Guessing Which Psychobiotics You Need
The research shows psychobiotics work—but only when you're taking the right strains for YOUR bacterial imbalances.
Our AIM Method combines comprehensive metagenomic testing (reviewed by Victoria, our in-house microbiologist) with personalised protocols that target YOUR specific deficiencies in psychobiotic bacteria.
We don't recommend generic psychobiotic supplements. We recommend specific strains when testing shows you need them.
Book a free 15-minute evaluation call to discuss your symptoms and whether testing could identify which psychobiotic species are depleted in your gut.
Book Your Free Evaluation Call
Putting It in Perspective
Eating well and supporting a healthy gut microbiome is one of the most powerful ways you can influence your mental health. What our grandmother's grandmother knew intuitively, we now have science to support—food truly is medicine.
Whether it's prebiotic vegetables feeding probiotic psychobiotics or simply nourishing your body on a deeper level, taking charge of your health is in your hands (and on your plate).
But when diet alone isn't enough—when you've been eating well, managing stress, and still experiencing anxiety, depression, or brain fog—it's time to test.
Testing reveals which psychobiotic species are depleted, which inflammatory bacteria are elevated, and which interventions will actually restore your gut-brain axis—not generic recommendations based on population studies.
Book Your Free Evaluation Call
Find Out Which Psychobiotic Bacteria YOUR Gut Is Missing
Psychobiotics are powerful—specific strains like B. longum 1714, L. helveticus, and Faecalibacterium prausnitzii can reduce stress, improve mood, and support cognitive function.
But taking psychobiotic supplements without knowing your bacterial balance is expensive guesswork.
At Prana Thrive, we use our AIM Method to identify which psychobiotic species are depleted, which inflammatory bacteria are driving symptoms, and which interventions will actually work for YOUR gut-brain axis:
Analyse — Comprehensive metagenomic testing reveals your psychobiotic bacterial levels (Bifidobacterium, Lactobacillus, Faecalibacterium), inflammatory bacteria, and functional capacity. Reviewed by Victoria (our in-house microbiologist) and me (after analysing over 2,000 microbiome tests).
Integrate — A personalised protocol designed for YOUR bacterial imbalances. If testing shows depleted B. longum, we might recommend B. longum 1714. If testing shows depleted Faecalibacterium, we'll focus on butyrate-supporting interventions. Not generic psychobiotic recommendations—targeted protocols based on your test results.
Monitor — Ongoing support with regular check-ins, protocol adjustments, and retesting to ensure the interventions are working. We track your progress for 3–6 months until your gut-brain axis is restored.
This isn't guesswork. It's precision.
We've helped over 2,000 clients improve their mental health by identifying which psychobiotic bacteria they're actually missing—not which supplements have the best marketing.
Book a free 15-minute evaluation call to discuss your symptoms, stress levels, mood challenges, and whether comprehensive testing is right for you.
We work with a limited number of clients each month to ensure everyone receives personalised attention. If you're ready to stop guessing which psychobiotics to take and get real answers about your bacterial balance, book your call now.
Book Your Free Evaluation Call
No pressure. No obligation. Just clarity on which psychobiotic bacteria YOUR gut actually needs.

