What Is Gut Dysbiosis?
Plus Associated Conditions
Author:
Amanda Ledwith, BHSc Naturopathy
Last Updated:
15 Jan 2026
Reading Time:
30 mins
Categories:
Gut Health
what-is-gut-dysbiosis
What You'll Learn
Gut dysbiosis simply means there is a microbial imbalance in your gut—most often within different populations of bacteria, but other microbes like yeasts can become imbalanced too.
How dysbiosis occurs:
Loss of beneficial bacteria (antibiotics, chemicals, dietary choices, stress)
Increase in pathogenic bacteria (gastro, food poisoning, parasites)
Low diversity (fewer bacterial species = fewer nutrients and metabolites produced)
Chronic stress (norepinephrine increases pathogenic bacteria)
Common symptoms:
Digestive: Constipation, cramping, diarrhoea, heartburn, gas, bloating
Skin: Acne, eczema, psoriasis, rashes
Mental health: Brain fog, anxiety, depression, difficulty concentrating
Systemic: Chronic fatigue, headaches, migraines, aching joints, food sensitivities
Associated conditions: IBS, ulcerative colitis, inflammatory bowel disease, type 2 diabetes, obesity, Parkinson's disease, heart disease, rheumatoid arthritis, multiple sclerosis, autism, Alzheimer's disease, chronic fatigue syndrome, coeliac disease, and more.
But here's what most people don't realise: You can eat more fibre, take probiotics, avoid processed foods, manage stress—but if you don't know which beneficial bacteria are depleted and which pathogenic bacteria are elevated, you're guessing. Testing reveals YOUR specific bacterial imbalances so you can target the right interventions.
Introduction
If you've ever suffered with digestive problems like cramping, constipation, diarrhoea, or grumbly gas, you'll know just how debilitating they can be. Not to mention embarrassing.
And while it's obvious these issues arise from your belly, have you ever wondered if your acne, chronic fatigue, or anxiety have something to do with your gut too?
My clients often wonder how these seemingly separate conditions are connected:
Digestive distress + brain fog … or
Bloating + anxiety … or
Constipation + chronic acne … or
Diarrhoea + exhaustion
The list goes on. And quite often a number of these symptoms arise together.
I treat so many people who are silently suffering with both digestive and non-digestive problems—symptoms they've been led to believe are completely unrelated. It's so common that it's often predictable.
But how are they related? The answer is deceivingly simple: gut dysbiosis.
In this article, you'll learn how your gut and your body are connected, what gut dysbiosis is (and what it's not), the signs and symptoms of gut dysbiosis, its causes, tests that work, and treatment options.
What Is Gut Dysbiosis?
Gut dysbiosis simply means there is a microbial imbalance in your gut. Most often within different populations of bacteria (as these are the most abundant), but other microbes like yeasts can become imbalanced too.
There are a number of ways that dysbiosis can occur:
When you lose beneficial bacteria in your gut—with antibiotics, chemicals, dietary choices, etc.
Gastro or infections from food poisoning or parasites may allow pathogenic bacteria to increase
You have low diversity
Chronic stress is a common cause
And so many more…
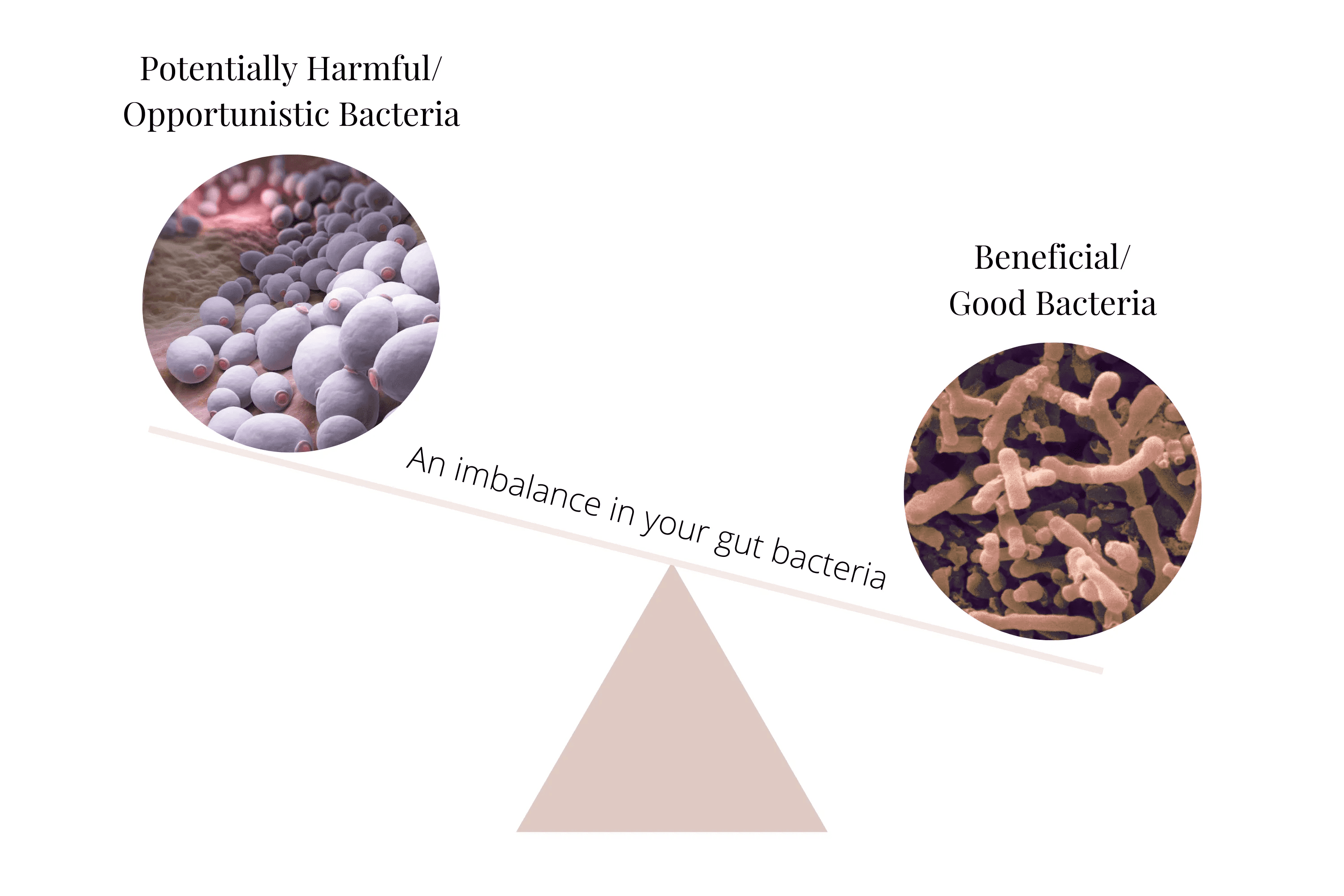
The majority of bacteria in your gut are actually "beneficial bacteria," meaning they will not cause you any harm and are of benefit to your health.
Some of these are called probiotic bacteria—there are also plenty that haven't earned this title but are definitely still beneficial.
There are also many groups of bacteria that need to be kept in balance by a thriving community of beneficial bacteria—and they will not cause harm. However, if their populations increase substantially, they can cause problems.
This situation is called gut dysbiosis.
It's All About Balance
(and Diversity)
A healthy and highly diverse gut will often house more than 1,000 different species of bacteria—living symbiotically in a fluid state of balance.
Along with balance (something we can see from your gut testing results), diversity is also a key indicator of gut health. This important diversity metric is included in comprehensive gut microbiome testing.
For most clients struggling with gut issues, we commonly see diversity scores in the range of the low 200s up to 600-ish—with the balance tipped toward (or very much all the way) into dysbiosis.
When in balance, our extensive community of bacteria work together in a complex and highly evolved microbial ecosystem.
They use the food we provide to exchange and excrete metabolites between each other—keeping one another in balance by default and contributing to our health and wellbeing in the process.
And an important part of this symbiosis is that we also benefit from their by-products and interactions too.
Our gut bacteria perform so many beneficial functions:
Help you maintain a healthy metabolism
Breakdown and digest your food
Make vitamins, minerals, and other beneficial nutrients
Maintain the integrity of the lining of your gut
Excrete the revered gut powerhouses SCFAs (short-chain fatty acids)
And so much more…
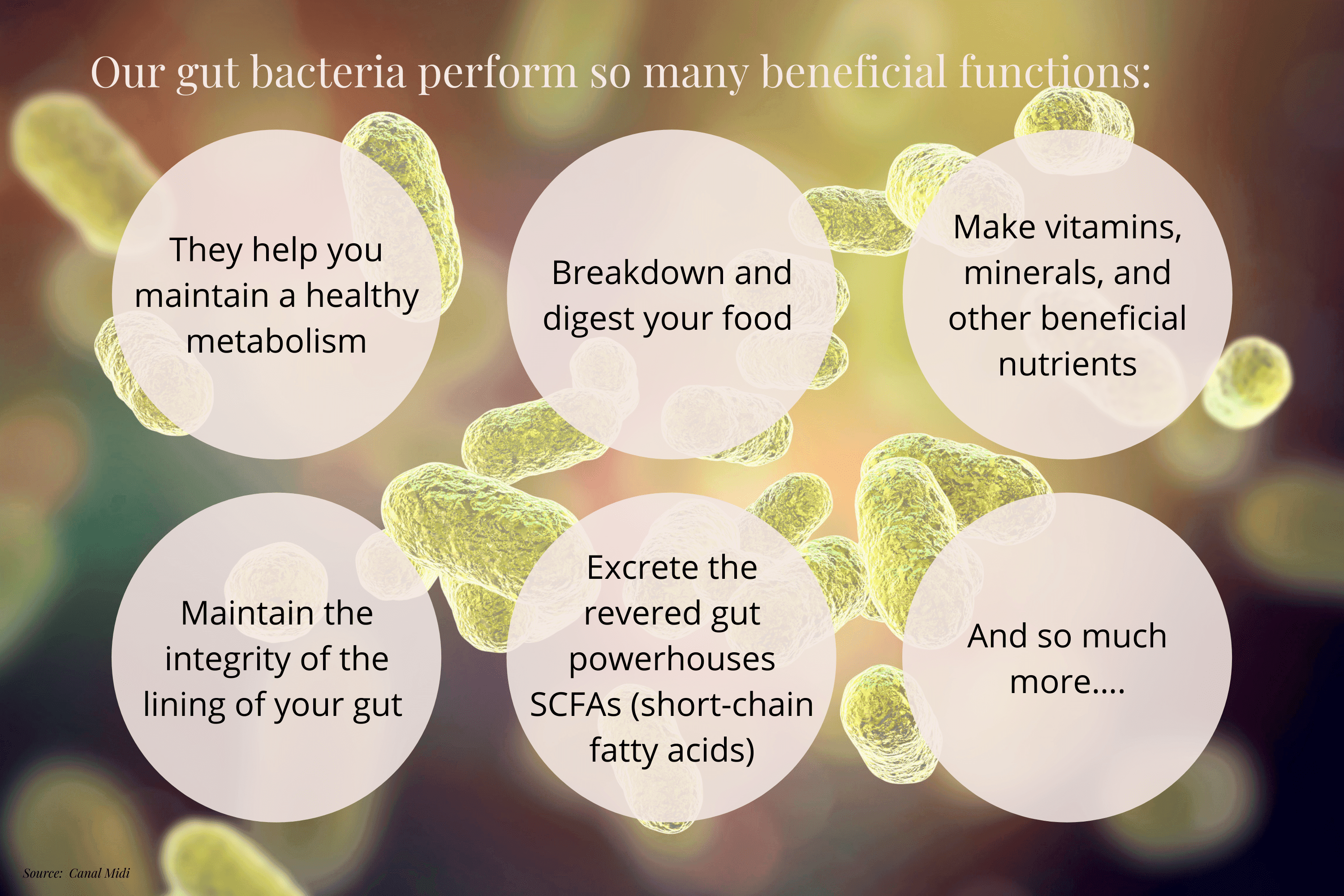
Ultimately, the silent activities of your gut bacteria are so important in our overall health that they've been recognised as an "organ." And so, it makes sense that you consider this thriving microbial organ along with your heart health, brain function, or physical fitness.
For example, let's say you decided you want to develop your physical fitness—what would you do? You'd include activities that you knew worked toward this goal.
You would change your habits to positively affect fitness—like limiting overeating poor-quality foods, becoming mindful of sedentary practices, signing up to a gym or taking a yoga class, and so on.
In a similar way, this process is not that much different for gut health. You need to do more of what brings you closer to your goal and less of what takes you farther away.
And gratefully, with the advent of gut microbiome testing, we have a pretty clear idea of what those things are:
You need to focus on building diversity within your gut microbiome—diversity brings a greater variety of nutrients and metabolites that you need
Within this diversity you need to foster a healthy balance—in favour of beneficial microbes rather than detrimental species
To be aware that everything you do impacts your microbes—because your gut microbiome is an organ and is connected with your lifestyle and choices, especially everyday food and diet decisions
So in concert with being an organ, bacterial metabolites play a crucial role in communication between our other organs—communicating with everything from your immune system, your hormones, and even your brain.
When we look at it this way, it makes perfect sense that when your gut bacteria are out of whack, the consequences are certainly far-reaching.
Read more: The Gut-Brain Connection: How Your Microbiome Affects Your Mood
Gut Dysbiosis Symptoms and Signs
It's because of this interconnectivity that gut dysbiosis causes a huge range of effects and a similarly huge range of signs and symptoms.
Including (but certainly not limited to) the following:
Digestive Symptoms:
Constipation
Cramping
Diarrhoea
Heartburn
Gas
Bloating
Food allergies, intolerance, or sensitivities
Skin Symptoms:
Acne
Skin conditions, rashes, dermatitis
Psoriasis
Eczema
Mental Health Symptoms:
Difficulty concentrating, brain fog
Anxiety
Depression
Systemic Symptoms:
Chronic fatigue
Inflammation and inflammatory conditions
Aching joints
Migraine
Headaches
Memory loss
Other Symptoms:
Hormonal disturbances
Candida overgrowth
Reduced immune function
Irritable Bowel Syndrome (IBS) and symptoms
Allergies
Asthma
Autoimmune conditions
Nutritional/vitamin deficiencies
… and the list goes on
But there is a common thread: reduction of gut lining integrity.
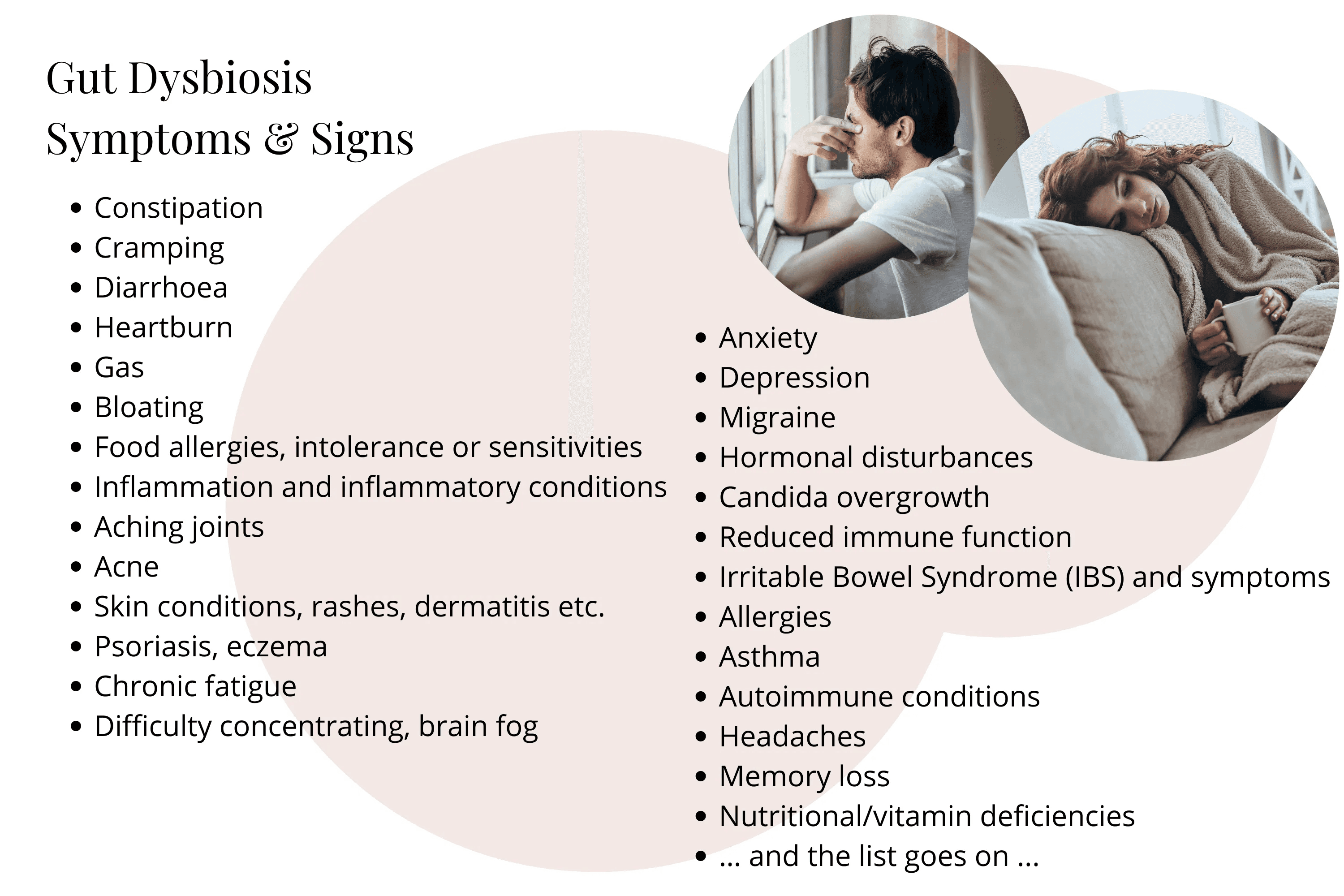
Dysbiosis is known to both cause and contribute to intestinal permeability. Often called "leaky gut," this inflammatory process refers to the loss of function of our vital gut protection barriers in the gut lining.
When the gut becomes leaky, antigenic substances like toxins, bacteria, and food breakdown products can enter your bloodstream, which triggers your immune system and results in the variety of symptoms we mentioned—such as nutrient malabsorption, autoimmune responses, brain fog, and fatigue.
Read more: Do You Have Leaky Gut? (Plus Warning Signs to Look For)
It really is a very long list—and it's growing.
Consequently, there's an equally large list of conditions that have dysbiosis connections.
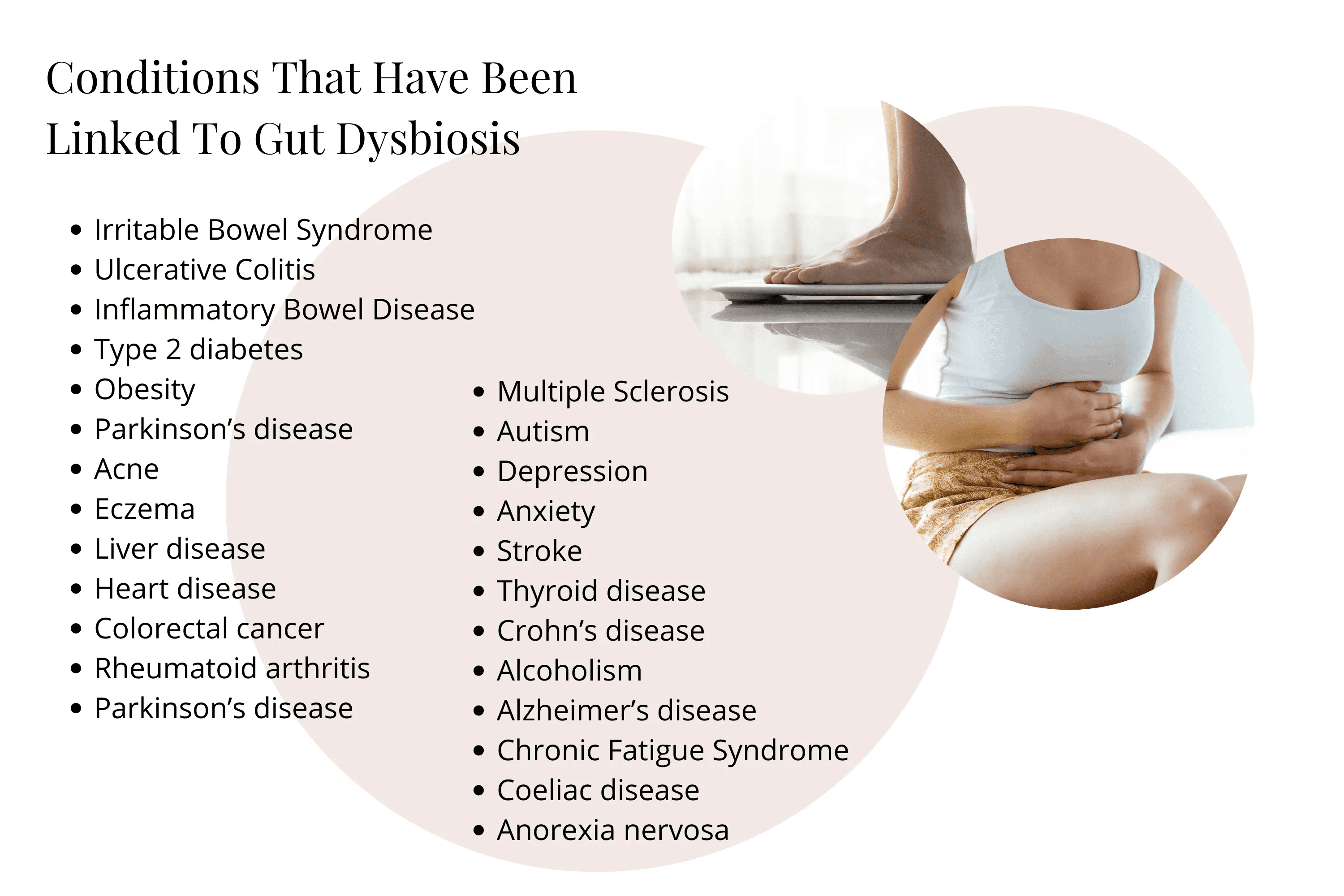
Conditions That Have Been Linked to Gut Dysbiosis
The following list includes just some of the enormous number of conditions that were once thought to be stand-alone illnesses but have been linked to gut dysbiosis.
It may surprise you to see how many of these are non-gut-related:
Digestive Conditions:
Irritable Bowel Syndrome
Ulcerative Colitis
Inflammatory Bowel Disease
Crohn's disease
Coeliac disease
Metabolic Conditions:
Type 2 diabetes
Obesity
Neurological Conditions:
Parkinson's disease
Multiple Sclerosis
Autism
Alzheimer's disease
Stroke
Mental Health Conditions:
Depression
Anxiety
Chronic Fatigue Syndrome
Anorexia nervosa
Skin Conditions:
Acne
Eczema
Cardiovascular Conditions:
Heart disease
Liver disease
Autoimmune Conditions:
Rheumatoid arthritis
Thyroid disease
Other Conditions:
Colorectal cancer
Alcoholism
Research has uncovered so much about how gut dysbiosis affects our health—but in many cases there is still uncertainty around which came first: the condition or the dysbiosis.
But what is now being more accepted is how our modern lifestyles, medical interventions, and just about everything can influence our gut balance.
Book Your Free Evaluation Call
Your Gut Dysbiosis Has a Specific Bacterial Pattern – But What Is It?
Gut dysbiosis isn't one-size-fits-all. Some people are depleted in Faecalibacterium prausnitzii (butyrate producer), others have elevated Proteobacteria (inflammatory), and some have low diversity across hundreds of bacterial species.
Our AIM Method uses comprehensive metagenomic testing to identify YOUR specific bacterial imbalances—not generic dysbiosis management.
We don't recommend generic probiotics and fibre supplements. We identify which beneficial bacteria YOU're depleted in and which pathogenic bacteria are elevated.
Book Your Free Evaluation Call
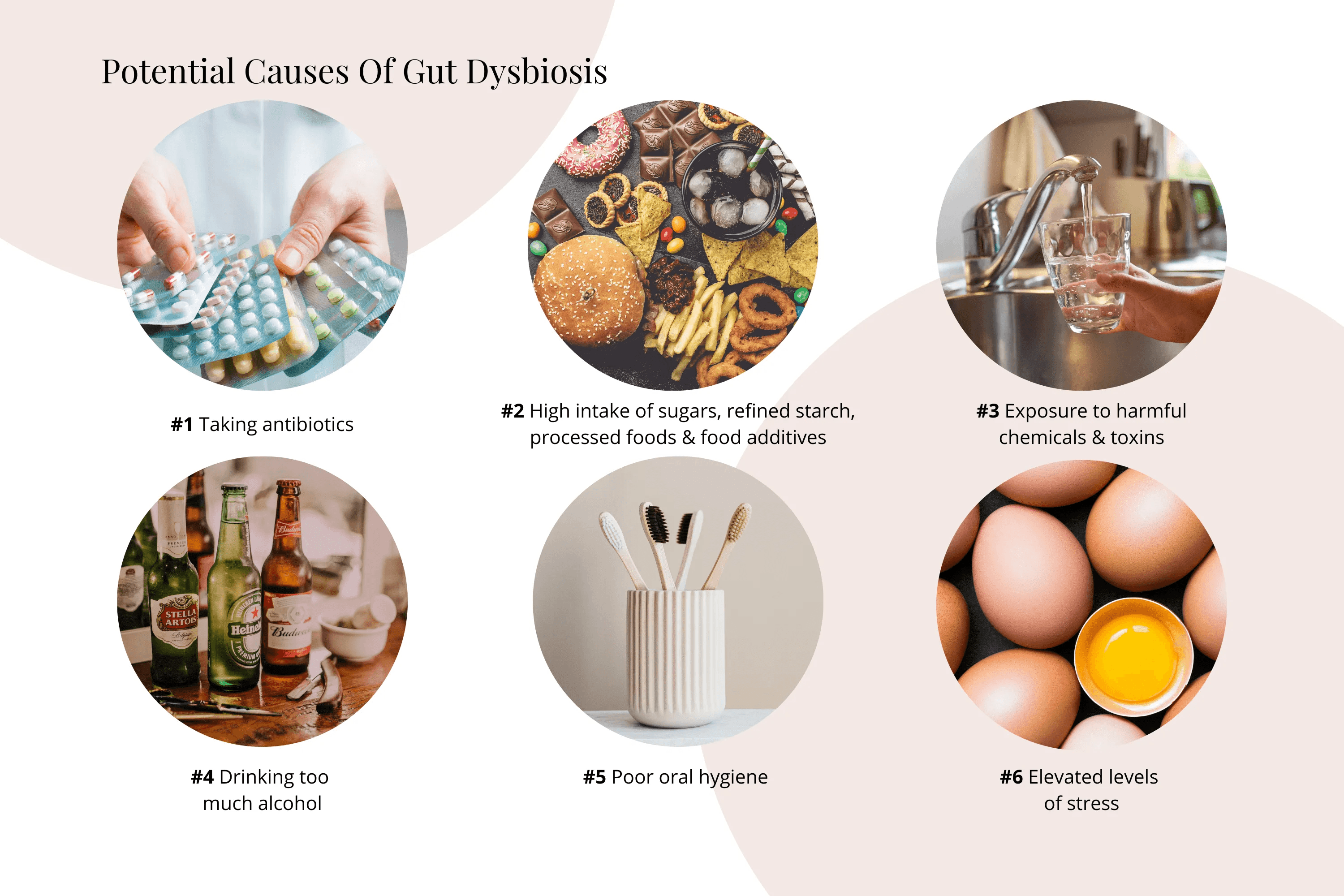
Potential Causes of Gut Dysbiosis
If you have gut dysbiosis, it could be as a result of any number of the following potential factors. And often these occur in combination to create a hostile environment for beneficial bacteria.
#1 Taking Antibiotics, Antibacterial Supplements, and Medications
Did you know that taking antibiotics for just a short period of time actually shifts your gut to an unbalanced state of being in the long term? In fact, you can be in a state of dysbiosis for months or even years.
Research has shown that taking antibiotics such as metronidazole and omeprazole affects upwards of 30% of your microbiome makeup, and this can last up to 4 years.
Clindamycin is another devastating culprit.
Specifically, when you take antibiotics you reduce the number and diversity of bacteria in your gut. Why does this matter?
As we said earlier, the less diverse your microbiome is, the more reduced your supply of the nutrients and metabolites they produce. But also your immune system becomes compromised, as 70–80% of your immune cells call your gut home.
Tip: Be cautious with antibiotic use as much as possible. Sometimes they are definitely absolutely necessary. If you must take an antibiotic, AFTER you've finished your course of antibiotics, take a high-quality probiotic to help repopulate your gut.
Read more: The Gut-Immune System Connection: How Your Microbiome Affects Immunity
#2 High Intake of Sugars, Refined Starch, Processed Foods, and Food Additives
What we eat feeds our microbes. And sugars, refined starch, processed foods, and many additives selectively feed non-beneficial bacteria.
With every mouthful of sugary drinks, poor-quality sweets, and ultra-processed packet foods, you contribute to dysbiosis—even if only short term. When these habits become an everyday habit, dysbiosis becomes normal.
And if you thought the new wave of artificial sweeteners were safe, think again…
Sucralose (Splenda), for instance, has been "reported" to be safe because most of it is not absorbed or metabolised in our bodies. But what about that microbial organ?
Animal research has shown that sucralose affects the makeup of bacteria in the gut. Sucralose has also been shown to increase the amount of inflammation-causing products (toxins) secreted by the gut bacteria. Other artificial sweeteners have also been shown to cause gut dysbiosis.
Tip: Limit your intake of refined sugar, flours, processed foods, and artificial sweeteners.
Read more: Best Foods for Gut Health: The Complete Evidence-Based Guide
#3 Exposure to Harmful Chemicals and Toxins
We are constantly exposed to chemicals—from our drinking water to the plastic microwave food containers we reuse. These unwanted substances not only harm our cells but can also be very harmful to our gut microbiome.
A major cause is through ingestion of foods treated with highly toxic pesticides and herbicides. Fruit, vegetables, and grains grown conventionally are coated in chemicals many times during their growth.
One of the most widely used pesticides, chlorpyrifos, has been shown to increase the concentration of bad bacteria in the gut. Though chlorpyrifos is no longer commonly used in the States and Europe, it is still commonly used in other parts of the world. So if you are consuming produce from other parts of the world, make sure you wash it thoroughly.
Tip: If you can, eat locally and organically. By eating locally and organically, you not only decrease your chances of ingesting harmful chemicals, you increase your nutrient intake by eating produce that is at its peak nutritionally.
#4 Drinking Too Much Alcohol
Studies show that drinking too much alcohol increases the number of predominantly non-beneficial bacteria like Proteobacteria and Fusobacterium in your gut. Notably, Proteobacteria and Fusobacterium have been linked to inflammation in the body.
Not to mention the myriad of detrimental liver, brain, and nervous system effects alcohol induces.
Tip: Limit your alcohol intake. If you already have gut dysbiosis related to drinking too much alcohol, take a prebiotic, as research suggests that this may help improve your gut microbiome.
#5 Poor Oral Hygiene
Not taking care of your teeth properly may not only lead to tooth decay and gum disease—it may also result in gut dysbiosis. Studies have found that periodontal or gum disease is dysbiosis of the oral microbiome. The harmful bacteria and parasites which have been associated with gum disease also lead to a change in the gut microbiome and inflammation of the fatty tissue and liver.
Tip: Make sure you brush your teeth twice daily. You could also try swishing your mouth with extra virgin coconut oil, as research has found that swishing your mouth with extra virgin coconut oil for about 10 to 20 minutes is as effective as chlorhexidine mouthwash in reducing gum disease-promoting bacteria.
#6 Elevated Levels of Stress
You probably already realise that your brain affects your stomach. For instance, when you just think about eating, your brain sends signals to produce digestive juices. Well, the connection goes both ways.
Your gut actually sends signals to your brain when it is in trouble. As a result, when you have a problem with your gut as occurs with gut dysbiosis, non-digestive symptoms such as anxiety can occur. Truly amazing.
Stress is similarly a huge culprit when it comes to gut health. One of the chemicals released when you are under a lot of stress is norepinephrine. Research has shown that norepinephrine released during surgery (a form of stress) increases the production of the bad bacteria Pseudomonas aeruginosa, which can contribute to gut dysbiosis and potentially infection. In addition, norepinephrine causes other non-beneficial bacteria to multiply or become more potent.
Tip: If you are under a lot of stress, engage in relaxation techniques such as meditation and deep breathing exercises to assist you in managing stress.
Testing for Gut Dysbiosis
So beyond symptom spotting, how can you tell if you have gut dysbiosis?
It's actually easier than you may have thought.
A simple faecal test gives you a picture of the number of good and "bad" bacteria in your gut.
Gut Microbiome Testing
This is a comprehensive gut microbiome profiling test we use with clients. Advanced DNA technology is used to isolate the bacterial genes that come from the gut bacteria in your sample.
This test gives us a clear picture of the exact percentage and ratio of different species and important groups of bacteria in your gut. Experienced practitioners can then interpret this information into a practical plan.
After analysing over 2,000 microbiome tests, Amanda develops personalised plans in conjunction with both testing results, any recent blood work necessary, client conditions, and of course their most prevalent symptoms.
Read more: Understanding Gut Microbiome Testing: A Key Component of Our Programs
What About GP Stool Tests?
I want to clear up some confusion about faeces or stool tests that are commonly used by a GP. I'm often asked what the difference is.
Basically, your GP will order a pathology stool test that only looks for a handful of bacteria, parasites, or helminths that are known gut pathogens—things like Salmonella, Campylobacter, Shigella, and typical parasites like Giardia, Dientamoeba, etc., which can be very helpful when you have an acute case of gastro.
But for more chronic conditions, gut microbiome profiling gives information on bacterial pathogens too but also includes the majority of the 1,000 species of bacteria living in your gut.
Additionally, it offers important information about their relative abundance (how many of them there are) and includes the hundreds of beneficial and symbiotic species that a standard pathology analysis will not provide.
In short: Gut microbiome testing offers a more comprehensive look at who is living in your gut and how they are coexisting together.
It's a mainstay in our testing regime with good reason.
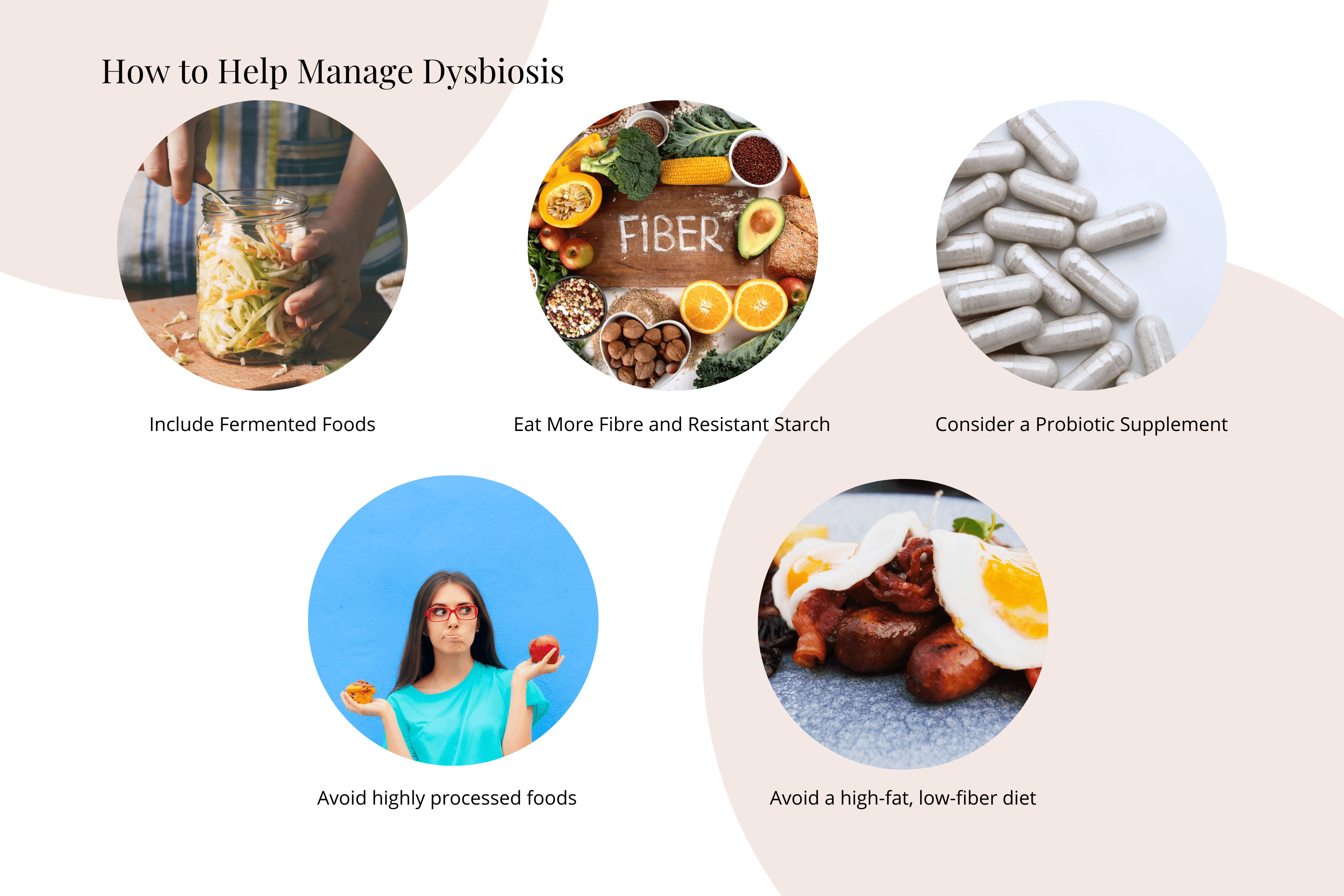
How to Help Manage Dysbiosis
Now that you know what gut dysbiosis is and what causes it, you may be wondering how you can tackle it.
There are a number of beneficial protocols that I recommend for clients based on their personal results and their conditions/symptoms. I commonly prescribe (where required) a unique combination of targeted high-quality practitioner-only herbal and nutritional medicines, high-strength probiotics, species-specific dietary modifications, and holistic lifestyle suggestions.
But here I will only outline simple practical support to begin to manage dysbiosis, as it's most beneficial for you and your microbiome that you work with an experienced practitioner to pinpoint your specific problem with guidance.
1. Include Fermented Foods
Eating fermented foods can be a helpful step toward gut health. Not only do they include naturally occurring probiotic bacteria, but new research suggests fermented foods also carry ready-to-go postbiotics like SCFAs and other beneficial bacterial metabolites. And most importantly, you're also eating the very food they need to continue to survive in your gut.
2. Eat More Fibre and Resistant Starch
Your beneficial gut bacteria need fibre to survive. By getting more fibre to where it's needed, you'll help build up your beneficial gut bacteria community and reap the beneficial metabolite benefits.
A few examples of fibre-rich foods include starchy tubers, vegetables, nuts, seeds, legumes, and fruit.
3. Consider a Probiotic Supplement
Investing in a high-quality probiotic supplement in order to increase the number of good bacteria in your gut can be beneficial if you are lacking in those specific species or strains.
As part of comprehensive testing programs, these probiotic bacteria are included in your report, and we offer tailored advice around which species would benefit you the most.
4. Avoid Highly Processed Foods
Are you a processed food junkie? If so, your eating habits could be contributing to gut dysbiosis. Processed foods typically contain a significant quantity of refined carbohydrates, sugars, fats, and artificial additives which, as we know, feed non-beneficial or "bad" bacteria.
A wholefood plant-predominant diet not only ensures you get a variety of prebiotic fibres and polyphenol-rich plant compounds for your gut bugs—it also naturally limits processed food intake.
And believe it or not, as your gut bugs change with your diet, so too will your tastebuds. As this happens, takeaway or processed foods don't actually taste the same as you remember.
5. Avoid a High-Fat, Low-Fibre Diet
The ketogenic diet with its high proportion of fats is all the rage now for weight loss, and I have worked with many clients who have definitely not felt better on it. So despite the seemingly radical weight-loss claims, it may not be a good idea for your gut microbiome.
Many species of non-beneficial bacteria love fat, so being on a ketogenic diet may not be a good idea, especially if you have gut dysbiosis. Studies have shown the keto diet to reduce some beneficial bacterial groups like Firmicutes and Bifidobacteria while increasing the less-beneficial Bacteroidetes and rotten-egg gas–producing Desulfovibrio spp.
A ketogenic diet does, however, also increase the powerful gut protector Akkermansia and can be a powerful protocol for specific health goals, but it is important to understand exactly what your food choices are doing to your gut.
Read more: How to Improve Gut Health Naturally: The Ultimate Guide
Book Your Free Evaluation Call
Stop Managing Dysbiosis Generically – Target YOUR Bacterial Imbalances
You've been eating more fibre, taking probiotics, avoiding processed foods—but your symptoms haven't improved. That's because dysbiosis isn't one pattern.
Our AIM Method combines comprehensive metagenomic testing (reviewed by Victoria, our in-house microbiologist) with personalised protocols that target YOUR specific bacterial deficiencies and overgrowths.
We don't recommend generic dysbiosis protocols. We identify which bacterial species you're depleted in and create targeted interventions.
Book a free 15-minute evaluation call to discuss your symptoms and whether testing could reveal which bacterial imbalances are affecting your health.
Book Your Free Evaluation Call
When Managing Dysbiosis Alone Isn't Enough: Why Testing Matters
You've been eating fermented foods, increasing your fibre intake, avoiding processed foods, taking generic probiotics—maybe you've even tried elimination diets, stress management, or expensive supplements.
But your symptoms haven't improved. Or maybe they improved briefly, then returned.
Here's what you need to understand: General dysbiosis management can be helpful—but only if you're addressing the specific bacterial imbalances driving YOUR symptoms.
Why General Dysbiosis Management Isn't Always Enough:
1. You Don't Know Which Beneficial Bacteria Are Depleted
Taking generic probiotics provides Lactobacillus and Bifidobacterium—but what if you're severely depleted in Faecalibacterium prausnitzii (butyrate producer critical for gut barrier integrity)? Or Akkermansia muciniphila (mucus layer protector)?
Eating more fibre feeds bacteria—but only if you HAVE those bacteria. If you're depleted in fibre-fermenting species like Faecalibacterium or Roseburia, eating resistant starch won't rebuild these populations quickly enough.
Without testing, you're guessing which beneficial bacteria are missing.
2. You Don't Know Which Pathogenic Bacteria Are Elevated
Fermented foods and probiotics increase beneficial bacteria—but if you have elevated Proteobacteria (Klebsiella, Proteus, Escherichia) producing inflammatory LPS, or Candida overgrowth, simply adding probiotics won't eliminate these overgrowths.
You might need targeted antimicrobials first, then rebuild beneficial species. Without testing, you don't know which pathogens are elevated.
3. Your Diversity Is Severely Low
If your diversity score is in the 200–400 range (healthy guts typically have 600+ species), you're missing hundreds of bacterial species and their metabolites—butyrate, acetate, GABA, serotonin, vitamins.
Generic probiotics provide 5–10 species. That's not enough to rebuild diversity when you're missing hundreds of species. You need targeted interventions to rebuild multiple bacterial families.
4. Antibiotic Damage Has Wiped Out Specific Species
If you've taken antibiotics in the past 6–12 months, you likely have severely depleted Bifidobacterium, Lactobacillus, and Faecalibacterium populations—with elevated opportunistic pathogens filling the void.
Generic probiotics might provide Lactobacillus—but if you're depleted in Faecalibacterium and Bifidobacterium too, you're only partially addressing the damage.
5. You're Feeding the Wrong Bacteria
Different bacterial species prefer different fibre types. Bifidobacterium thrives on inulin, Faecalibacterium prefers resistant starch and pectin, Akkermansia feeds on mucin.
If you're eating inulin-rich foods but you're depleted in Faecalibacterium and elevated in Klebsiella, you might be feeding pathogenic bacteria more than beneficial species—worsening dysbiosis.
What Testing Reveals
When Victoria reviews comprehensive metagenomic test results for clients managing dysbiosis, she identifies:
Which beneficial bacteria are depleted (Faecalibacterium, Bifidobacterium, Akkermansia, Lactobacillus, Roseburia)
Which pathogenic bacteria are elevated (Klebsiella, Proteus, Escherichia, Candida, Streptococcus)
Diversity scores (How many species are you missing? Are you in the 200s or 600s?)
Functional capacity (Is your microbiome producing butyrate? SCFAs? Are inflammatory metabolites elevated?)
Antibiotic damage patterns (Recent antibiotic use? Which species were wiped out?)
This information allows us to create a targeted protocol:
Specific antimicrobials if pathogenic overgrowths present
Targeted probiotics for YOUR depletion pattern (Faecalibacterium, Bifidobacterium, Akkermansia)
Specific prebiotics that feed the bacteria you're rebuilding (resistant starch for Faecalibacterium, inulin for Bifidobacterium)
Gut barrier repair if Faecalibacterium severely depleted (butyrate, L-glutamine, zinc carnosine)
The Bottom Line
If you've been managing dysbiosis for 6–12 months with fermented foods, probiotics, fibre, and stress management—but your symptoms haven't improved—the problem isn't that these interventions don't work. It's that you don't know which bacterial imbalances YOU have.
Testing shows exactly which beneficial bacteria are depleted, which pathogens are elevated, and which interventions will address YOUR specific dysbiosis.
To Recap
Gut dysbiosis is an imbalance in the bacterial community in your gut. It can result in a number of digestive and non-digestive signs and symptoms, including constipation, diarrhoea, anxiety, and depression. Additionally, gut dysbiosis is linked to a huge number of conditions, including Crohn's disease, type 2 diabetes, and colorectal cancer, to name a few.
And it may be caused by a number of factors, including drinking too much alcohol, taking antibiotics, and poor dental hygiene. The most accurate and comprehensive way to know if you have gut dysbiosis is comprehensive gut microbiome testing.
If you suspect you have gut dysbiosis, we can help you organise testing.
Book Your Free Evaluation Call
Find Out Which Bacterial Imbalances Are Driving YOUR Dysbiosis
Gut dysbiosis isn't one pattern. Some people are depleted in Faecalibacterium prausnitzii, others have elevated Proteobacteria, and some have low diversity across hundreds of bacterial species.
At Prana Thrive, we use our AIM Method to identify which bacterial imbalances are driving YOUR symptoms and create targeted protocols—not generic dysbiosis management:
Analyse — Comprehensive metagenomic testing reveals your diversity score, which beneficial bacteria are depleted (Faecalibacterium, Bifidobacterium, Akkermansia), which pathogenic bacteria are elevated (Klebsiella, Proteus, Candida), and functional capacity (butyrate production, inflammatory metabolites). Reviewed by Victoria (our in-house microbiologist) and Amanda (after analysing over 2,000 microbiome tests).
Integrate — A personalised protocol designed for YOUR bacterial imbalances. If testing shows depleted Faecalibacterium, we use targeted butyrate support, resistant starch, and gut barrier repair. If Proteobacteria elevated, we use specific antimicrobials to reduce LPS-producing bacteria, then rebuild beneficial species. Not generic probiotics and fibre—targeted protocols based on your test results.
Monitor — Ongoing support with regular check-ins, protocol adjustments, and retesting to ensure your beneficial bacteria are rebuilding, pathogenic bacteria are reducing, and diversity is increasing. We track your progress for 3–6 months until your symptoms resolve.
This isn't generic dysbiosis management. It's precision.
We've helped over 2,000 clients restore their gut health by identifying which bacterial species are depleted—not by recommending generic probiotics and fibre supplements.
Book a free 15-minute evaluation call to discuss your symptoms, gut health history, and whether comprehensive testing is right for you.
We work with a limited number of clients each month to ensure everyone receives personalised attention. If you're ready to stop guessing which bacterial imbalances are driving your dysbiosis and get real answers about YOUR microbiome, book your call now.
Book Your Free Evaluation Call
No pressure. No obligation. Just clarity on which bacterial species YOUR gut is missing.

