The Gut-Immune System Connection
Author:
Amanda Ledwith, BHSc Naturopathy
Last Updated:
22 Jan 2026
Reading Time:
XX mins
Categories:
Gut Connections
gut-immune-connection
What You'll Learn
Your gut houses 70-80% of your immune cells, making gut health fundamental to immune function. The gut-associated lymphoid tissue (GALT) works with your microbiome to orchestrate immunity.
Key immune structures in the gut:
Peyer's patches — Monitor bacterial populations and prevent pathogenic growth
Mesenteric lymph nodes — Filter antigens and coordinate immune responses
Gut mucosal epithelium — Single-cell barrier translating information to immune cells
IgA-secreting plasma cells — Produce antibodies that neutralise bacterial and viral toxins
How gut bacteria support immunity:
Produce short-chain fatty acids (SCFAs) like butyrate that fuel immune cells
Maintain gut barrier integrity (preventing leaky gut)
Train and regulate immune cell responses
Create antimicrobial compounds that control pathogens
Compete with harmful bacteria for resources
Signs of compromised gut-immune function:
Recurring infections (colds, flu, UTIs)
Slow wound healing
Autoimmune symptoms
Chronic inflammation
Food sensitivities and allergies
Why testing matters: Comprehensive microbiome testing reveals which immune-supporting bacteria are depleted, which inflammatory species are elevated, and whether gut barrier integrity is compromised—allowing targeted protocols to restore immune function.
Did you know, the strength of your immune system, the balance of your microbiome and health of your gut are all deeply interconnected?
We tend not to associate our gut with our cold-fighting ability, but actually, it's role is crucial for our immunity.
If you struggle with recurring illness or seem to catch whatever bug is going around, it's absolutely important you understand the gut-immune connection.
Knowing how to manage and support your immune system from the gut can change your health. And your life!
Simply put, your immune system is mostly in your gut. It is estimated your gut houses a massive 70 – 80% of your immune cells!
So being mindful of your microbiome is so much more than just watching your waistline, your health depends on it.
Tending to your ecosystem of trillions, who in turn regulate, monitor and orchestrate the cells responsible for the strength of your immunity (and much more) is a fundamentally important immune-boosting strategy.
And it is as profoundly life-changing as it is simple.
The Key to Gut – Immune Health
Essentially, you need to nourish the hundreds of different microbial species supporting your immune system for balance and positive health.
Typically when we take so-called immune boosting supplements or consume foods said to be good for your immune system, we believe we're increasing the circulating immune cells in our blood. So they can be ready to fight lurking viruses or pathogens we may encounter.
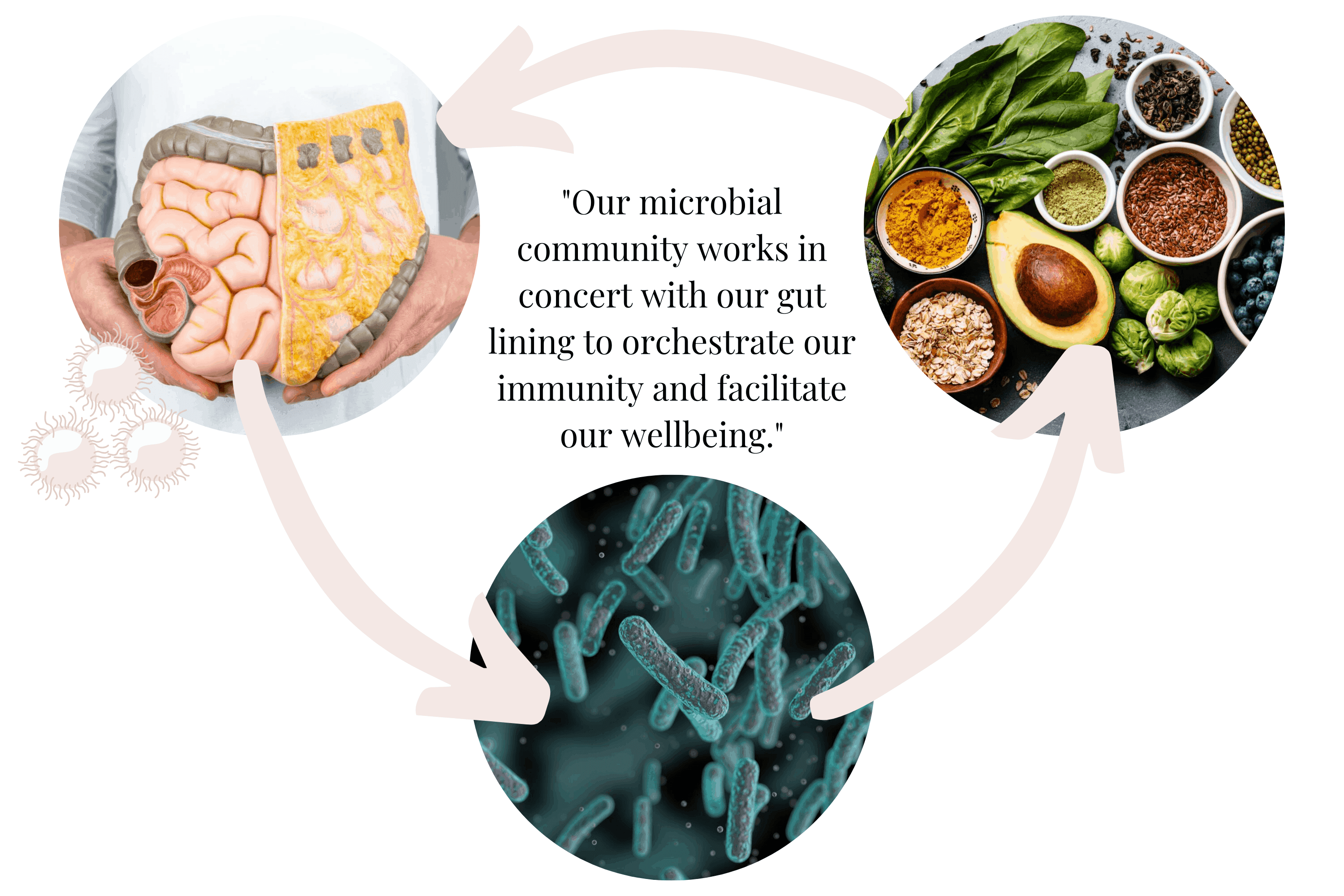
While this does occur, it's only part of the story. The big picture is far more complex and epically more synergistic.
It is now known, our microbial community works in concert with our gut lining to orchestrate our immunity and facilitate our wellbeing. Understanding how you can influence the strength of your immune system and how it works will help you support your gut health and of course your general wellbeing.
Immune System Basics
So we can better understand the role our gut plays, first let's take a quick look at how our immune system as a whole works to protect us.
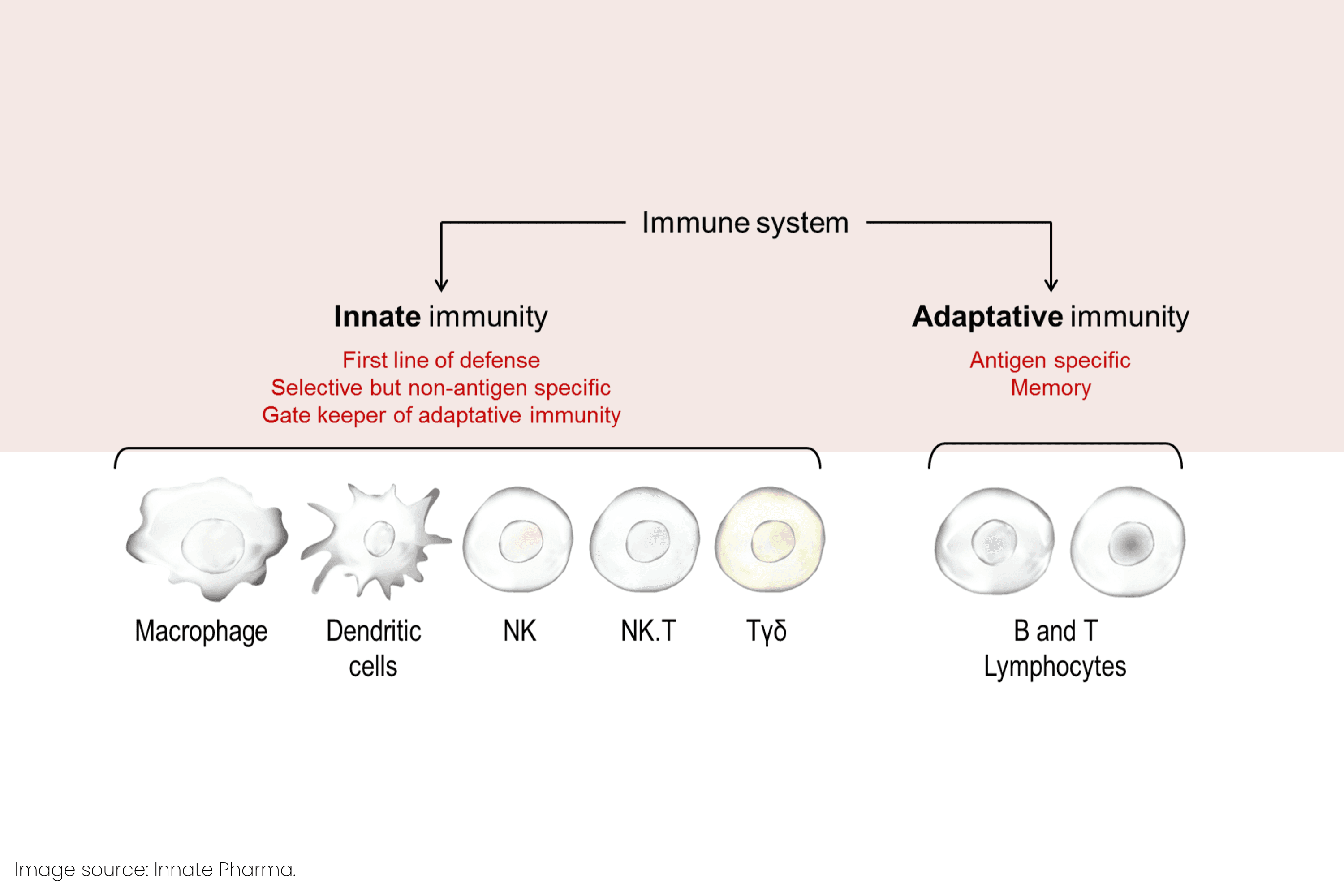
There are thought to be two types of immune response.
Non-specific (or innate) – A general first-line of defense approach focused on keeping threats out.
Specific (or adaptive) – Focused and targeted complex immune responses which develop when non-specific immunity is unable to adequately contain the threat.
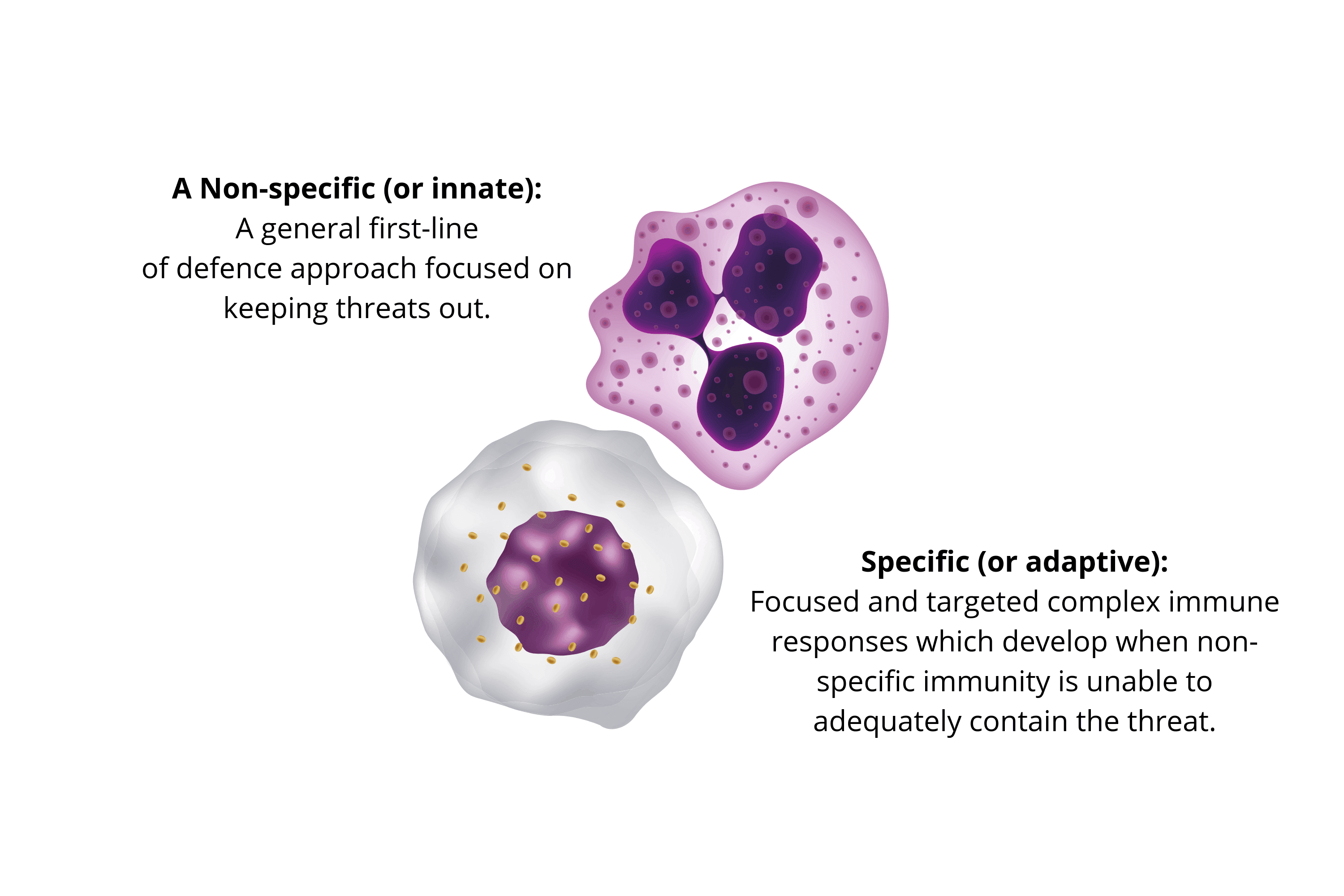
Innate immunity comprises both physical and chemical barriers, like our skin, mucus membranes, stomach acid etc. But also general patrolling cellular responses.
General inflammatory cells are constantly on the lookout for threats and when they encounter one, act fast to neutralise or destroy any foreign or damaged cells. These cells also provide invaluable information (or reconnaissance) for further adaptive immune responses.
Adaptive responses are highly complex and form the basis of what we call our immunity. Specialised cells function to remember invaders (who carry antigens) and can invoke a specific response to known pathogens or damage. This response is mediated by lymphocytes. A type of white blood cell with numerous functions that is critical for our immunity.
Antigens are parts of substances foreign or toxic material encountered in the body. Some examples include bacteria, viruses, parasites, venom, certain proteins in food and even blood components from other individuals. Antigens act as biochemical flags to invasion and response from our lymphocytes.
Interestingly, the antigenic load provided by the food we eat plays a massive role in shaping our immunity. Our intestines encounter more antigens than any other part of the body. We will discuss antigens in further detail later, as our immune response to antigens can determine our health.
Immune Cells Within the Gut
To understand how our immune system is connected with the gut, let's explore the mechanics of the gut in more detail.
Your gastrointestinal tract, or gut, is roughly 5m in length, has an approximate surface area of 32 square metres and is home to an estimated 100 million neurons.
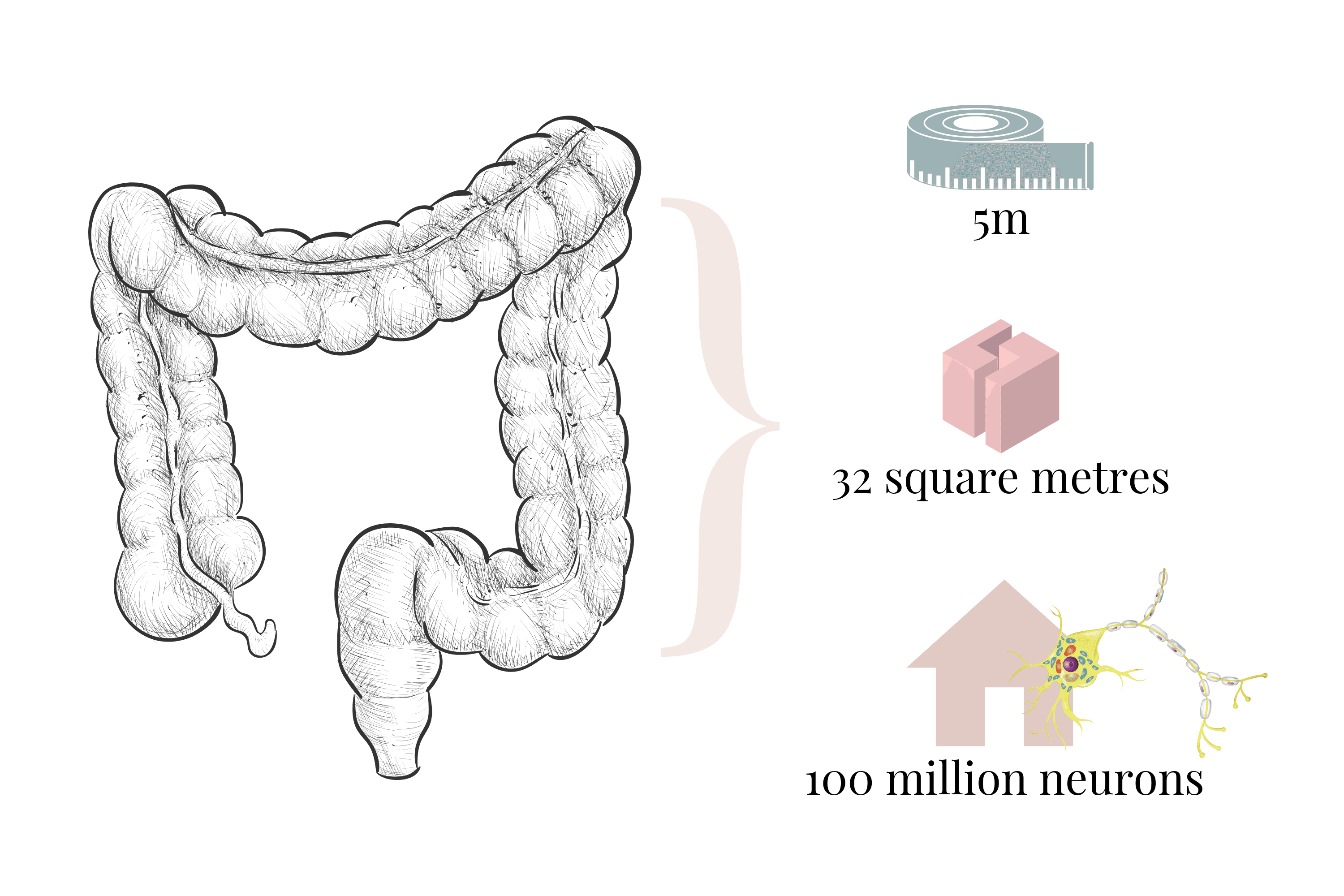
And of course billions of beneficial microorganisms. Your gut microbiome.
Within this microbe dense, neuron-rich, multi-layered collagen tract lies your largest immune organ in the body, the GALT.
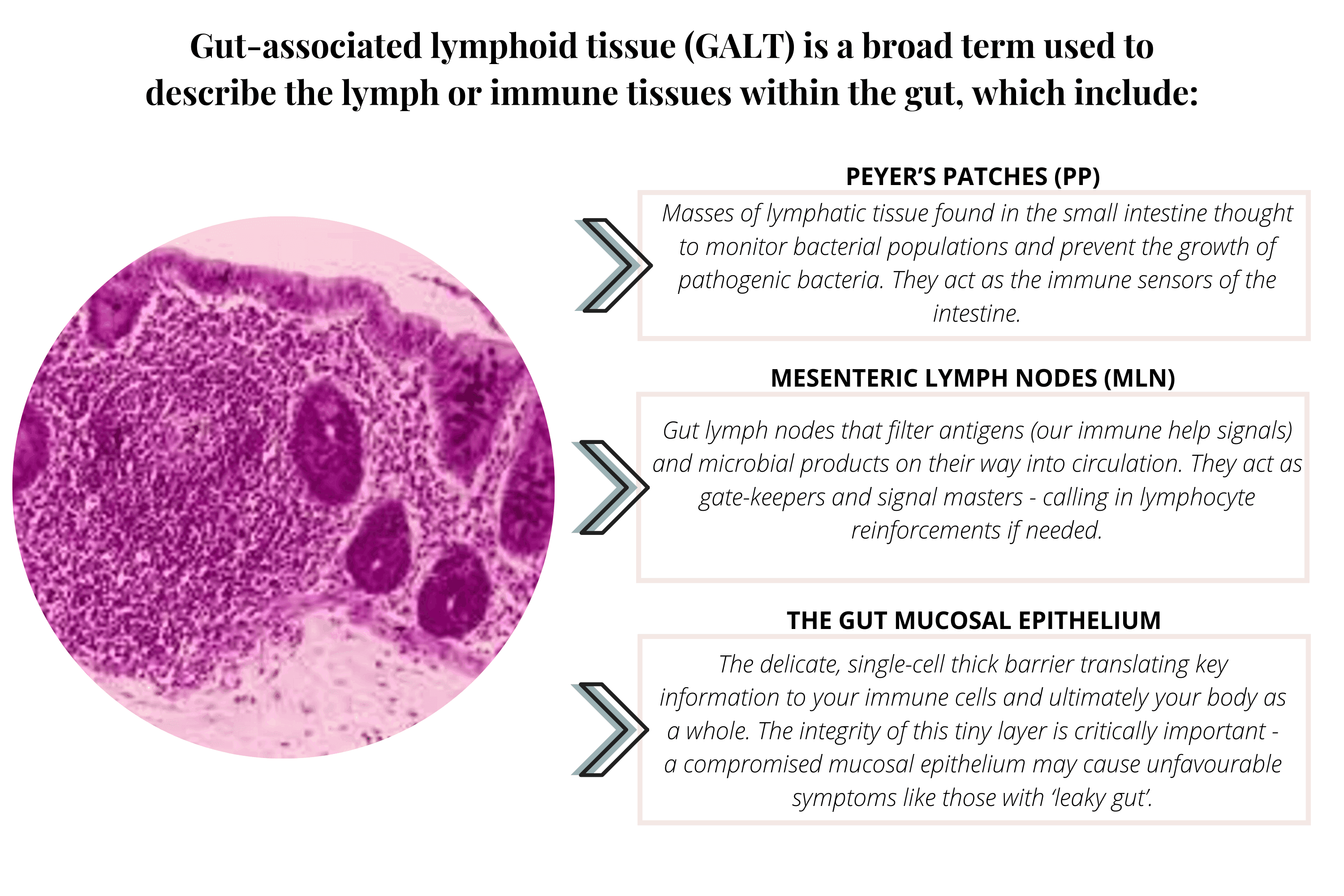
Gut-associated lymphoid tissue (GALT) is a broad term used to describe the lymph or immune tissues within the gut. These fundamentally important lymphatic tissues are interwoven with arteries, veins and nerve fibres creating a tight immune network all working with your greatest health in mind.
You may have heard some of these, which include:
Peyer's patches (PP) – Masses of lymphatic tissue found in the small intestine thought to monitor bacterial populations and prevent the growth of pathogenic bacteria. They act as the immune sensors of the intestine.
Mesenteric lymph nodes (MLN) – Gut lymph nodes that filter antigens (our immune help signals) and microbial products on their way into circulation. They act as gate-keepers and signal masters – calling in lymphocyte reinforcements if needed.
The gut mucosal epithelium – The delicate, single-cell thick barrier translating key information to your immune cells and ultimately your body as a whole. The integrity of this tiny layer is critically important – a compromised mucosal epithelium may cause unfavourable symptoms like those with 'leaky gut'.
These tissues act as signalling sites, providing neural and immune feedback using our diet and microbiome to create both generalised and threat-specific immune cells.
Understandably, our immune cells arising from these tissues are responsible for many functions including controlling, eliminating or signalling for threats.
White blood cells are abundant in the gut and form part of the inflammatory response, these include plasma cells, dendritic cells, activated T-cells, macrophages and many more. Living in your GALT, generally, these cells envelop threats and trigger a larger or more specific immune response.
IgA-secreting plasma cells operate out of the gut, providing secretions to coat the gut mucosal epithelium (our epithelial cell layer mentioned above) and function as a primary defense against infection. IgA is produced by B-cells and T-cells in the gut and acts to neutralise bacterial and viral toxins but also to stop them adhering to the intestinal wall.
This alone is a fundamental reason to nourish your gut and learn how to support these amazing cells as they are key to your health. There are a dizzying array of cellular interactions taking place every second of our lives, the lengths these cells go to for our ultimate health is as humbling as it is complex.
Foundational Immune Functions of Your Gut Lining & Leaky Gut
Immune cell pathways are closely controlled and absolutely dependent upon the single cell layer of the intestinal epithelium. This tiny barrier is all that stands between our food/microbes and our body systems. The integrity of your gut lining is crucially important.
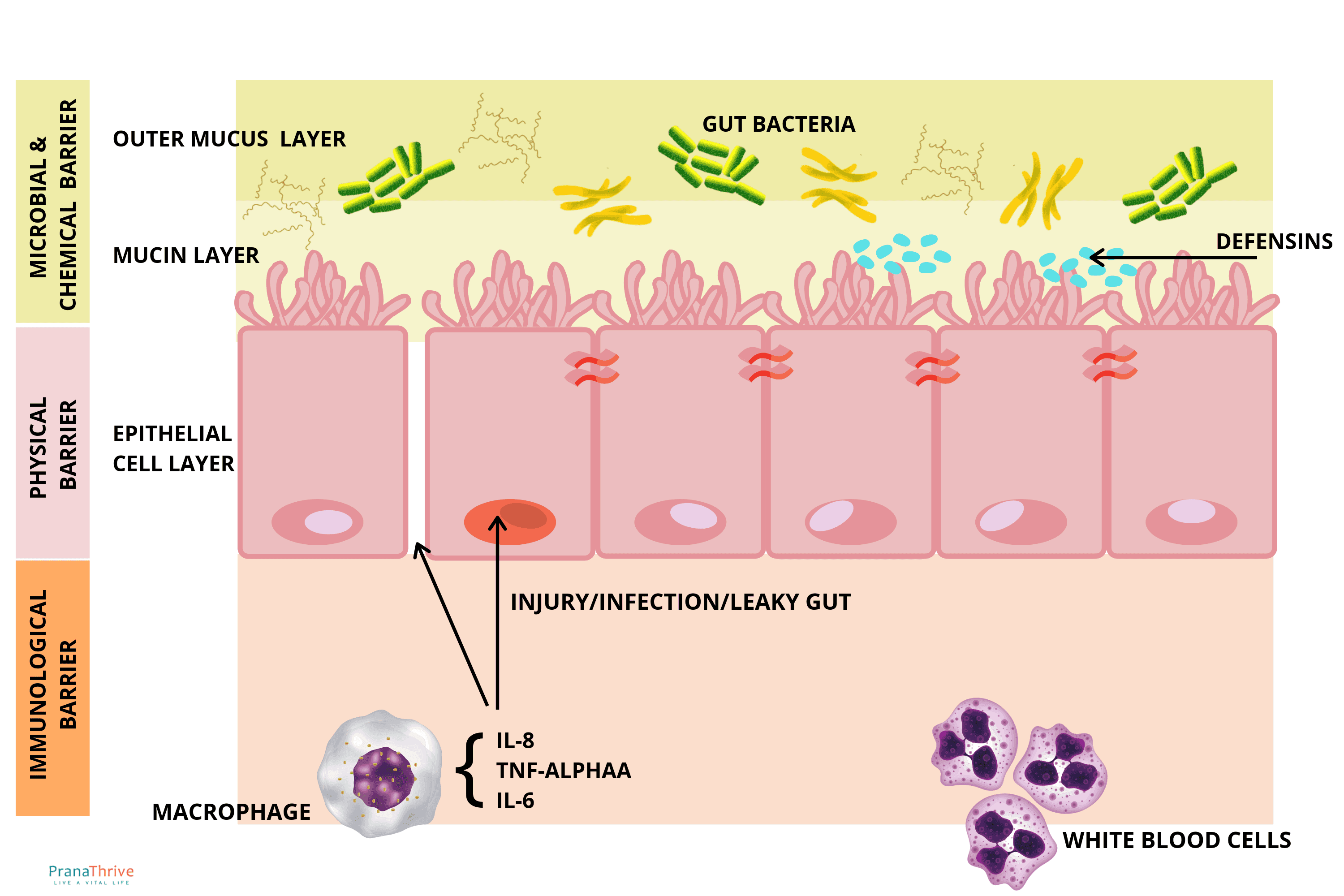
Some other gut lining immune functions include:
Mucin layer – Supporting a layer of mucus that can interact and trap bacteria. Produced by both certain bacteria and too specialised cells.
Defensins – Supply of antimicrobial proteins secreted by special cells in the intestinal folds.
Epithelial cell microbe sensing – The gut lining can secrete factors e.g., IL-8, TNF-alpha, IL-6 that alert other cells of microbial presence, instigating the recruitment of white blood cells.
Consequently, deficiencies or defects in gut mucosal epithelial function contribute to inflammation and associated conditions, such as leaky gut and IBS. Here microbiome balance is key.
As we discussed, gut epithelial cells function to provide a protective mucus layer. This layer serves to both feed beneficial bacteria (like Akkermansia) and harbour non-ideal microbial populations. Whether the beneficial microbes outnumber the non-ideal depends on what you feed them (and you).
This is just one critical role your gut microbial community have on your immunity.
Why Bacteria Are Important for a Healthy Immune System
Before we look further at bacterial influence on the immune system, let's talk about antigens, or our antigenic load.
Understanding what an antigen is and how they affect our immunity will make the picture a lot clearer.
As we briefly covered, the term antigen is used to describe parts of substances that our immune cells can recognise and create a memory bank from. They may be a fragment of DNA or genetic material retrieved from an eliminated microbial threat, a portion of a protein from food or even a toxin.
To help us understand, immunologists explain that antigens act in a kind of tiny lock and key mechanism. Imagine a bacterial cell as a microscopic tic-tac shape with lots of Y shapes covering the surface. Like a hairy caterpillar.
Now imagine these Y-shaped antigens coming across much bigger blob shaped white blood cells with little triangle shapes on the surface. The antigen Y and the white blood cell triangle 'fit' each other and trigger a reaction in the white blood cell, sometimes to engulf and eliminate the bacteria, other cells may produce antibodies encoded to remember this particular threat.
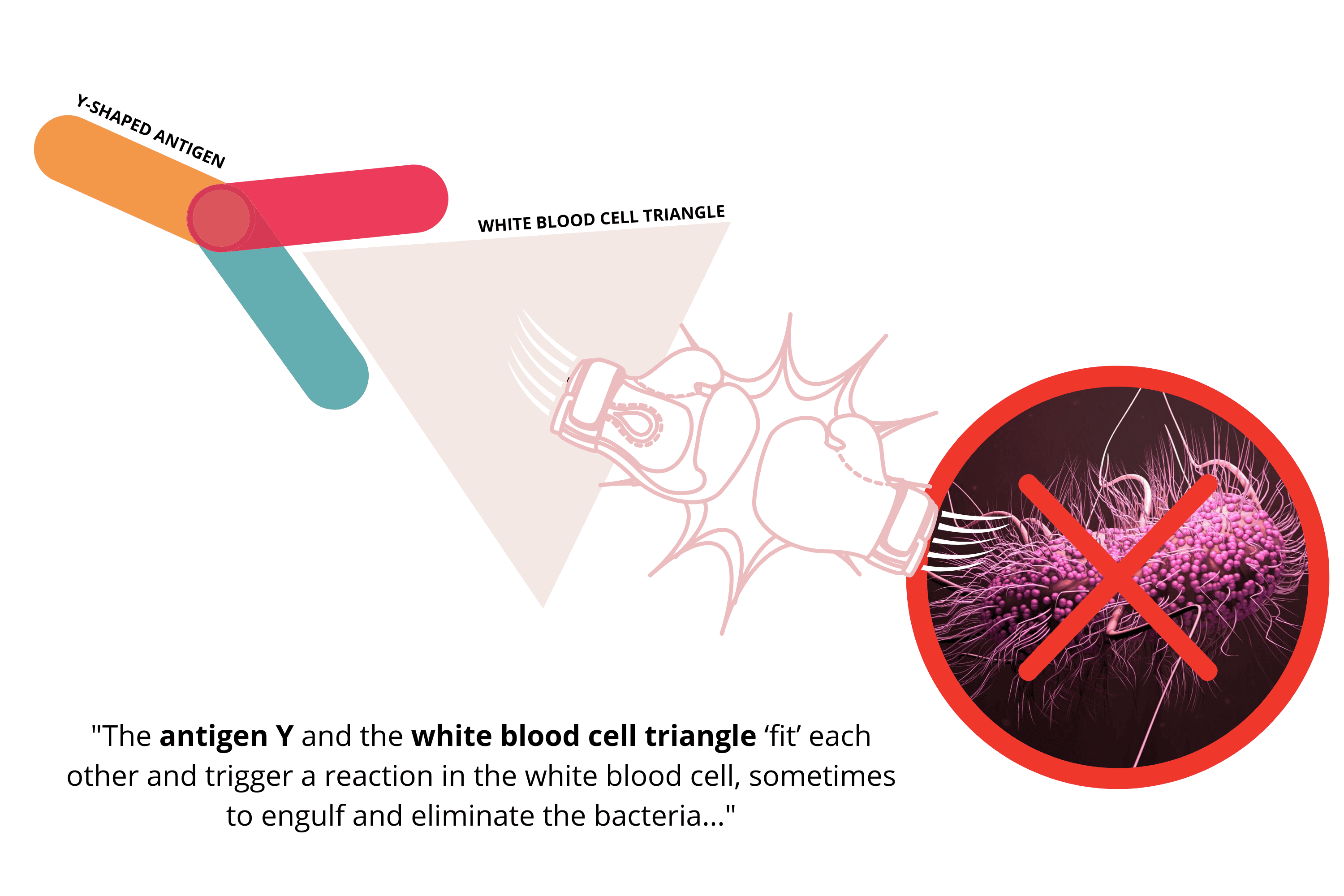
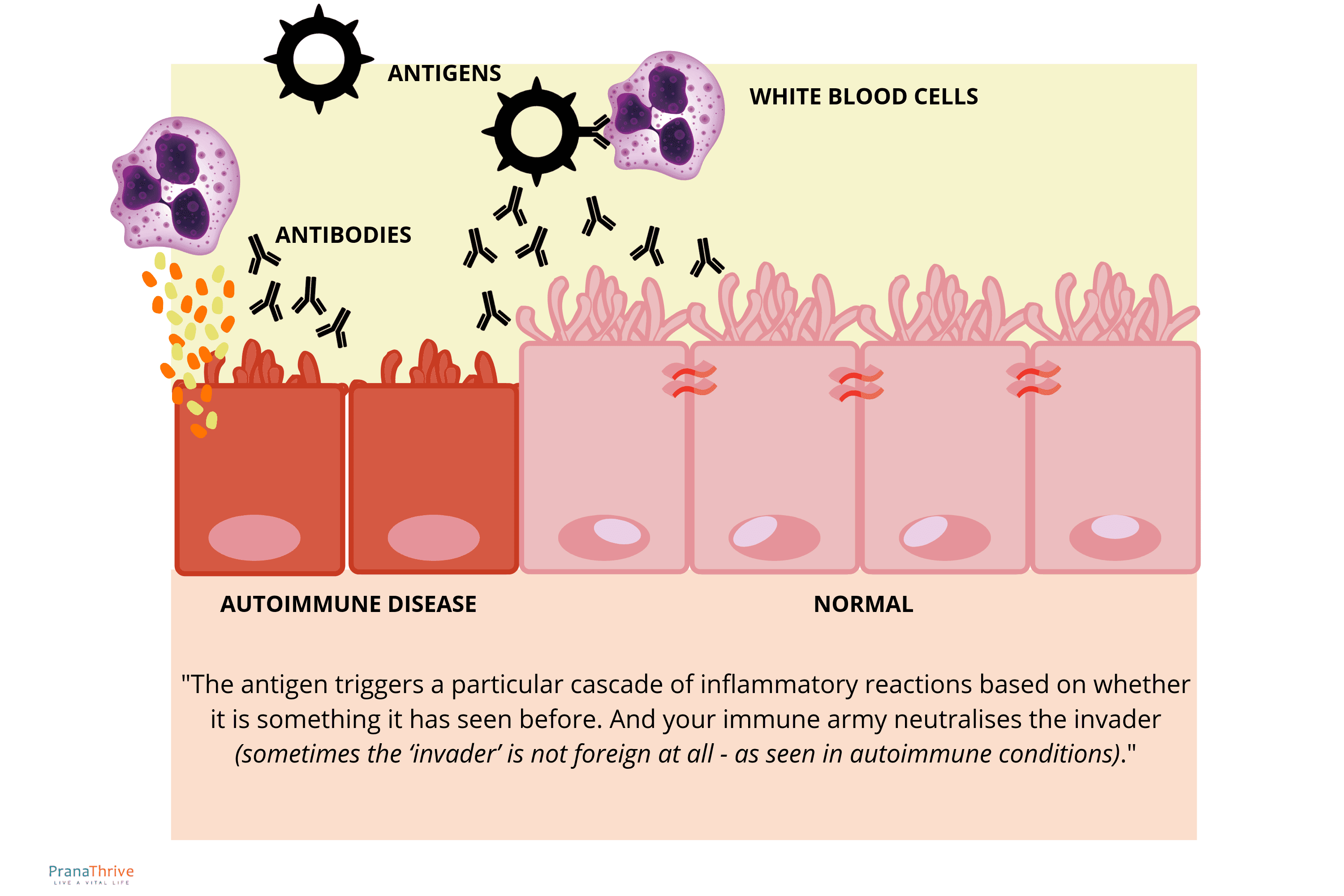
Essentially, this is how your body beings to mount an immune response based on antigenic properties. The antigen triggers a particular cascade of inflammatory reactions based on whether it is something it has seen before. And your immune army neutralises the invader (sometimes the 'invader' is not foreign at all – as seen in autoimmune conditions).
In this way your body interacts with all the microbial species living on your body but particularly in your gut. Similarly, bacterial species interact with each other forming a harmonious and unimaginably complex ecosystem of interactions based on chemical properties, genetic transfer, food availability and more.
This is where the importance of the diversity and composition of your microbiome come into play.
🔬 VICTORIA'S EXPERT INSIGHT
"When I review microbiome test results, I'm specifically assessing the bacterial species that directly support—or compromise—immune function. This goes far beyond just looking for pathogens.
What I assess for immune function:
1. SCFA-producing bacteria Short-chain fatty acids (butyrate, propionate, acetate) are the primary fuel for immune cells and gut barrier maintenance. When I see depleted Faecalibacterium prausnitzii, Roseburia, Eubacterium, and Anaerostipes species, I know the client's immune cells are literally starving for energy. These are the first bacteria I look to rebuild.
2. Gut barrier integrity markers Akkermansia muciniphila is critical for maintaining the mucus layer that protects the gut lining. When Akkermansia is absent or severely depleted (which I see in most clients with immune issues), the gut barrier is compromised—allowing bacterial fragments (LPS) to cross into the bloodstream and trigger systemic inflammation. This is the mechanism behind leaky gut.
3. Inflammatory bacterial patterns Elevated Proteobacteria (especially Klebsiella, Citrobacter, Enterobacter) produce lipopolysaccharide (LPS)—a potent inflammatory trigger. When I see elevated LPS-producing bacteria alongside depleted anti-inflammatory species, I know the immune system is in a chronic state of activation. This explains symptoms like fatigue, brain fog, joint pain, and recurring infections.
4. IgA and secretory immunity markers Certain bacterial patterns suggest compromised secretory immunity—the IgA-producing cells that protect mucosal surfaces. This explains why some clients get every cold that goes around, have recurring sinus infections, or struggle with UTIs. Testing reveals whether the bacteria that support IgA production are present.
5. Histamine-producing bacteria For clients with histamine intolerance symptoms (allergies, skin reactions, anxiety), I check for elevated histamine-producing bacteria. These species directly drive allergic-type immune responses, and reducing them often resolves symptoms that antihistamines only mask.
The critical insight: Your immune system isn't weak—it's responding to the bacterial signals it's receiving. Testing reveals whether those signals are coming from beneficial bacteria supporting immune function, or inflammatory species triggering chronic activation. Targeted protocols can shift this balance."
— Victoria, Microbiologist
Immune, Nutrient and Bacterial Interaction
Certain bacterial populations support the health and integrity of your gut lining and nutrient uptake more than others. Their abundance is dependent on the availability of food favourable food sources.
Short chain fatty acids (SCFAs) are a great example of how bacterial nutrient processing impacts immunity. SCFAs are created when particular microbes ferment plant fibre – or resistant starch.
Butyrate, a type of SCFA, is not only used as an energy source for our colon cells but also affects immune responses through the cytokine (inflammation cascade messenger) profile production of helper T cells and helps to maintain epithelial layer integrity preventing microbes escaping from our gut.
Butyrate is produced by numerous bacterial communities including bifidobacteria, Faecalibacterium, Eurotium, Anaerostipes and Roseburia. When fed enough fibre these bacteria directly support our gut health and immunity. As do many others in innumerable ways.
In this way, our microbiome supports our gut lining, our immune system and creates our white blood cell memory bank slowly building our immunity from birth using all the bacteria, viruses, food and other substances which we have been exposed.
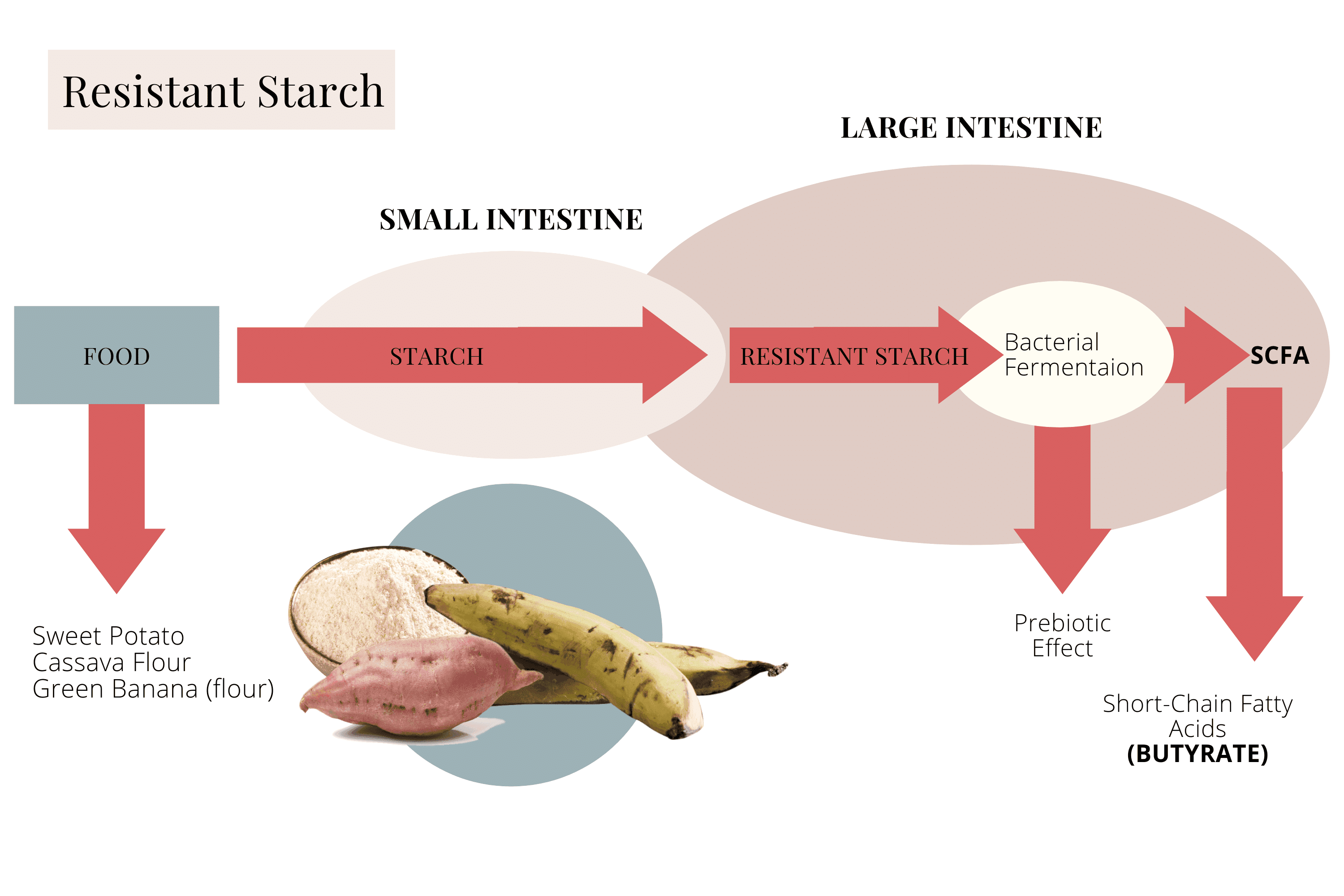
Image Source: How To Improve Gut Health Naturally: The Ultimate Guide
Gut Immune Connection From Birth
The way in which we come into the world has a tremendous impact on our gut and immune health.
It is now commonly held that babies born naturally have vastly different microbiome profiles than those born via C-section.
Vaginal birth produces a microbiome more closely resembling their mother's gut bacteria (not vaginal) whereas environmental bacteria from the hospital and skin microorganisms colonise C-section babies.
This has been seen to have effects lasting for the first year of life. A crucial window in the development of both the microbiome and immune system.
A lack of beneficial microbes in early life has been linked to many diseases, particularly autoimmune conditions such as asthma, diabetes and allergies. This is further compounded by maternal and infant antibiotic exposure, whether you were breast or formula fed and many other factors.
It is even thought that antibiotic exposure in the womb may lead to decreased ability to fight viral infection as a child. Certain T-cell responses are suppressed and direct affect our antiviral immunity.
Building a healthy microbiome from birth shapes our lifelong immunity and health. How your body reacts to the bacteria you carry around in your gut, whether they are seen as friend or foe, creates the basis of your health and disease.
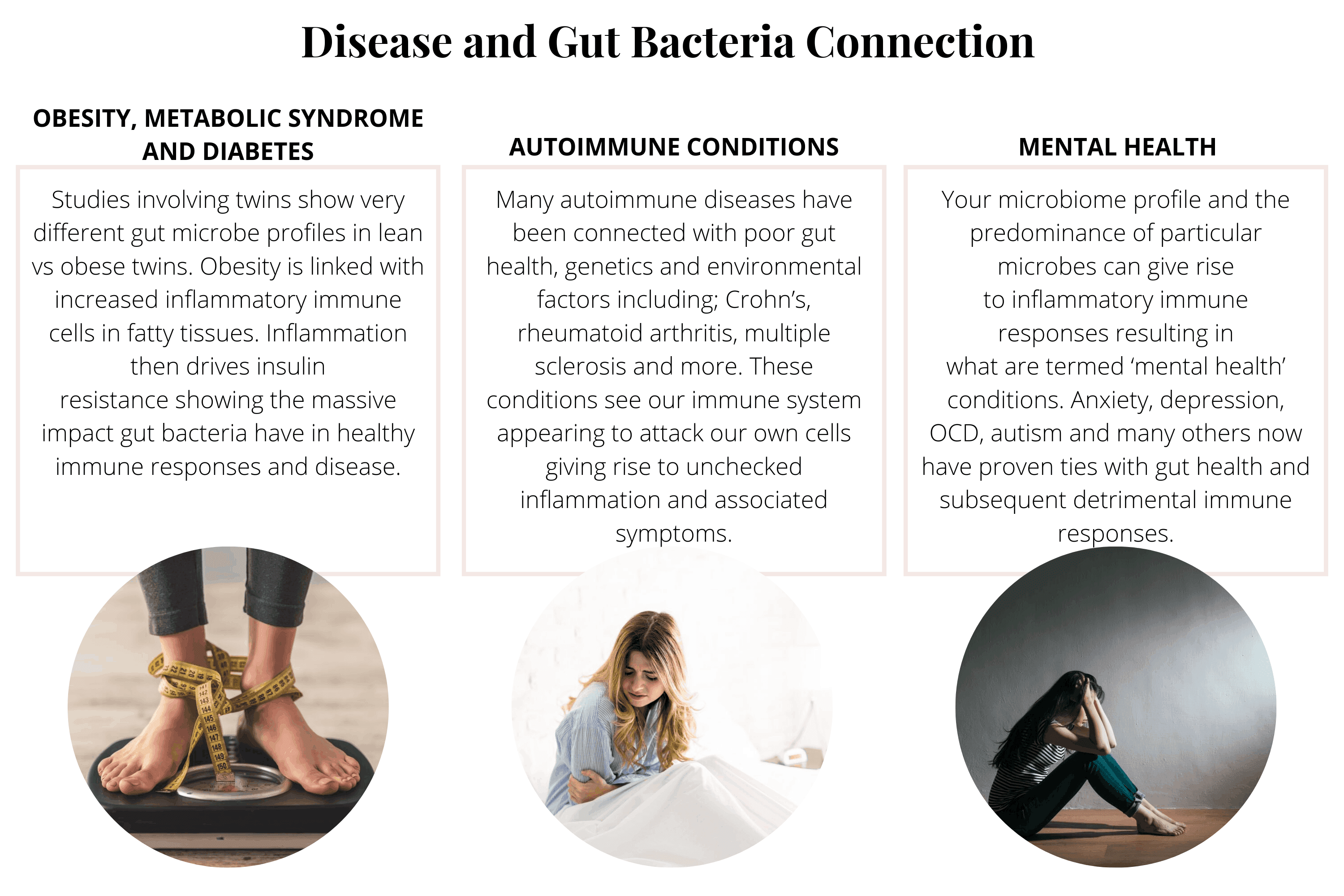
Disease and Gut Bacteria Connection
While we all seem to blame our genetics for our immunity, health or lack thereof (it undoubtedly plays a role – read more about Nutrigenomics here), there is a far more empowering position to view disease.
The connection between our gut microbes and disease has been clearly demonstrated in numerous studies worldwide. Let's visit the most common diseases and examine their immune connection.
Obesity, metabolic syndrome and diabetes – While excess nutrient-poor caloric intake and processed food consumption play a huge role, numerous studies involving twins show very different gut microbe profiles in lean vs obese twins.
This is further supported in research involving faecal transplant for obesity in both human and animal models. Obesity is linked with increased inflammatory immune cells in fatty tissues. Inflammation then drives insulin resistance showing the massive impact gut bacteria have in healthy immune responses and disease.
Autoimmune conditions – Many autoimmune diseases have been connected with poor gut health, genetics and environmental factors including; Crohn's, rheumatoid arthritis, multiple sclerosis and more. These conditions see our immune system appearing to attack our own cells giving rise to unchecked inflammation and associated symptoms.
Mental health – Your microbiome profile and the predominance of particular microbes can give rise to inflammatory immune responses resulting in what is termed 'mental health' conditions. Anxiety, depression, OCD, autism and many others now have proven ties with gut health and subsequent detrimental immune responses.
Taking care of brain and neurological health starts in the gut and is mediated by bacteria and associated immune pathways.
Gut health and microbiome balance affects so many areas of our lives and health all mediated by our immune system.
By now you should be getting a pretty good idea about how and why the strength of your immune system is connected with good gut health.
Without a diagnosis of a gut-associated condition, it's a good idea to understand some of the earlier signs of gut dis-ease and imbalance. Or better yet get your gut health and microbiome scientifically tested!
So you can work towards a state of balance before your body starts sending serious disease alert signals.
Signs Your Gut Bacteria Are Unhealthy
There seem to be as many signs of an unhealthy microbiome as there are illnesses. It is thought that a reason for this may lie in the fact that disease in any form originates from the gut. Or dysbiosis of the gut microbiome.
The following symptoms have been associated with unhealthy gut bacteria. If you display any of these symptoms it is important to check in with your preferred health provider or experienced holistic practitioner to create a personalised treatment plan.
Gut symptoms – Typical gut signs include bloating, gas, constipation and diarrhoea. These even present as an embarrassing combination of all of the above. Digestive issues such as heartburn, bad breath and tooth decay can also point to microbiome distress.
Read more – What is Gut Dysbiosis (And Associated Conditions)Skin symptoms – Breakouts, eczema, uneven skin tone, dark circles and acne have all been implicated in a sluggish and inflamed gut. Taking care of your skin is far better tackled from the inside out. Swap your creams out for the SCFA benefits of fibre for your microbiome to ferment!
Read more – Gut Skin Connection (All You Need To Know)Brain symptoms – Neurological signs such as brain fog, memory loss, headaches, mood changes all point to inflammation and an immune response. Poor diet, stress, environmental factors and genetic predisposition all play a role in brain health. It's not all in your head!
Read more – Gut Brain Connection And How It Affects Your Mood
These are just a handful of the many symptoms of an unhealthy gut. If you are looking for a better understanding of your gut health and microbiome or genetic testing, we offer comprehensive and personalised programs to help you improve your gut immune function.
Achieving gut health and a better microbial balance may seem complex and overwhelming but there are simple steps you can take to start healing your gut little by little every day.
Read more – How to Improve Gut Health Naturally: The Ultimate Guide
Diet – A great place to start is to make sure you are eating lots of wholefood fibre (especially for your SCFA producing bacteria to feast on). Plant-focused, wholefood meals provide a great source of health-supporting nutrients, minerals and fibre to begin to shift the balance in favour of beneficial microbes. Not to mention the benefit of plant-based phytochemicals such as polyphenols act to both inhibit and encourage various gut bacteria all aiding in balance and immune support. Remember to include your good fats, probiotics and fermented foods too!
Lifestyle – There are many everyday changes you can make to support your immune system through gut healing. Simple swaps such as reducing the chemical load you are exposed to in your home and personal care products play a massive role. Reducing stress, exploring outdoors and getting some sunshine all support your health and wellbeing via your microbiome. And don't forget adequate chemical free-water hydration and sleep!
Learn – One of the most effective ways to improve your gut health is to learn about gut health. Like you are doing now. Educating yourself, your friends, family and anyone who will listen goes a long way to changing how we see our food, our health and our planet.
Quite simply natural gut healing and support is a return to simple, wholesome and natural living not long ago lost to our fast-paced, processed, stressed out lifestyles.
As we begin to heal our gut and support our microbial friends and our immune systems better health has no choice but to come along for the ride.
Summary
Let's quickly recap what we have covered:
Your immune system is primarily located in your gut – and the majority of immune stimulating antigens are in the food that you eat
Immune cells all work together to create a state of health in a complex array of pathways and feedback mechanisms – some cells acquire a memory for threats
Disease can often be traced to gut and microbiome imbalance mediated by immune responses and nutrient deficiencies
Gut immune health begins at birth – we are the sum of all our microbial experiences
There are as many signs of an unhealthy gut and there are illnesses and the immune system governs them all
Simple and natural steps can assist you in restoring the balance of your microbiome and achieve a healthier and stronger immune system
Book Your Free Evaluation Call
Stop Guessing Why Your Immune System Is Struggling - Test Your Gut
You've tried immune-boosting supplements. You've eaten more vitamin C. You've been told your blood work is "normal." But you're still getting sick frequently, struggling with allergies, or dealing with autoimmune symptoms—because no one has looked at where 70-80% of your immune system actually lives.
At Prana Thrive, comprehensive gut microbiome testing reveals the bacterial patterns driving your immune issues—not just whether pathogens are present, but whether the bacteria that support immune function are depleted.
Our AIM Method:
Analyse — Comprehensive microbiome testing reveals SCFA-producing bacteria levels (the fuel for immune cells), gut barrier integrity markers (Akkermansia, zonulin), LPS-producing inflammatory bacteria, histamine-producing species (for allergy patterns), and secretory immunity support. Every report workshopped by Amanda (2,000+ analyses, extensive experience with immune-related conditions) and Victoria (microbiologist who specifically assesses immune-supporting bacterial patterns).
Integrate — A personalised protocol designed to restore immune function from the gut. If SCFA-producing bacteria are depleted, we rebuild them with specific prebiotics and dietary interventions. If inflammatory bacteria are elevated, we reduce them with targeted antimicrobials. If gut barrier integrity is compromised (leaky gut), we repair it. If histamine-producing bacteria are driving allergic responses, we address the bacterial source. Not generic immune supplements—targeted interventions based on YOUR microbiome.
Monitor — Ongoing support with regular check-ins, protocol adjustments based on your symptoms and immune response, and retesting at 3-4 months to track bacterial shifts. We monitor SCFA-producing bacteria restoration, inflammatory marker reduction, gut barrier improvement, and immune symptom resolution. Immune restoration is measurable—we track the changes that matter.
This isn't symptom management. It's targeted protocols based on comprehensive testing that reveals what's actually driving your immune issues.
We've helped over 2,000 clients understand their gut-immune connection—identifying which bacterial species are compromising immune function and creating targeted protocols to restore balance.
Book a free 15-minute evaluation call to discuss your immune concerns and whether comprehensive gut testing is right for you.
We work with a limited number of clients each month to ensure everyone receives personalised attention and microbiologist-reviewed protocols. If you're ready to stop managing immune symptoms and address the root cause in your gut, book your call now.
Book Your Free Evaluation Call
No pressure. No obligation. Just clarity on whether your gut bacteria are contributing to your immune issues.
Because your immune system is only as strong as your gut.