Understanding Gut Microbiome Testing
A Key Component of Our Gut Health Programs
Author:
Amanda Ledwith, BHSc Naturopathy
Last Updated:
19 Jan 2026
Reading Time:
XX mins
Categories:
Gut Health
gut-microbiome-testing
What You'll Learn
Gut microbiome testing identifies which bacteria, fungi, and other microorganisms are in your gut—revealing imbalances that may be contributing to digestive issues, autoimmune conditions, and mood disorders.
Advanced testing methods in Australia:
16S rRNA sequencing (NGS): Identifies and quantifies gut microbial species with high accuracy
Shotgun metagenomic sequencing: Comprehensive snapshot including non-rRNA organisms like fungi, functional information, and antibiotic resistance genes
What comprehensive testing reveals:
Overall diversity (200–800+ bacterial species on average)
Balance across phyla (large microbiome groups)
Beneficial bacterial levels (Akkermansia, Lactobacillus, Bifidobacterium, Faecalibacterium)
Troublemaker bacterial levels (opportunistic pathogens)
Inflammatory markers and metagenomic data (SCFAs, vitamins, harmful metabolites like LPS)
Why testing matters:
Identifies root causes conventional pathology testing misses
Guides targeted interventions (not generic protocols)
Tracks progress with retesting at 3–6 months
Every test workshopped with Amanda and Victoria to assess diversity, dysbiosis patterns, beneficial/troublemaker bacteria levels, and metagenomic markers—then used to build personalised treatment plans.
Have you found yourself struggling with persistent digestive issues despite trying various remedies?
From dietary changes to supplements, you've explored numerous avenues, yet the discomfort persists.
You're not alone in this struggle.
Digestive concerns are increasingly common, affecting millions worldwide. Whether it's bloating, irregular bowel movements, or unexplained discomfort, these issues can significantly impact your quality of life.
But what if there's more to the story than just dietary choices and lifestyle factors?
What if the key to unlocking your digestive health lies within your gut microbiome?
Welcome to our world of gut microbiome testing, a revolutionary approach we use every day that goes beyond conventional gut health diet advice.
In this article, we'll delve into the significance of gut microbiome testing and its pivotal role in personalised health programs.
We will:
Explore the science behind PCR vs. culture techniques
Unravel examples of advanced testing methods used in Australia
Discover how our naturopaths harness this technology to tailor effective treatment plans
If you're ready to uncover the best tool we know of to establish the root cause of your digestive woes, read on.
Because when it comes to your wellbeing, knowing your unique microbiome numbers makes all the difference.
The Significance of Gut Microbiome Testing
Research has shown that an imbalance in the gut microbiome, known as dysbiosis, is linked to a myriad of health issues, including digestive disorders, autoimmune conditions, and even mood disorders like depression and anxiety.
Gut microbiome testing offers experienced practitioners a deeper insight into the root cause of these issues—the gut microbiome imbalances.
By analysing the composition of your gut microbiome, we use microbiome testing to identify specific bacterial groups and species that may be contributing to your symptoms.
In many cases, we find abnormalities that conventional pathology testing misses.
The two most common methods used in gut microbiome testing are PCR (Polymerase Chain Reaction) and culture techniques.
While culture techniques have traditionally been used to identify specific bacteria and are still used by a number of testing companies, PCR results offer a more comprehensive and accurate assessment of microbial communities.
In the next section, we'll delve into the differences between PCR and culture techniques, shedding light on why PCR is often preferred in modern microbiome testing.
PCR vs. Culture Techniques: Understanding the Difference
While both commonly used testing methods have their merits, they also come with their own set of limitations.
Traditionally, culture techniques were the go-to method for identifying bacteria in the gut. This approach focuses on finding a specific list of pathogens. It requires that a handful of petri dishes are inoculated with stool sample and grown in a lab incubator to mimic human body conditions, 37℃ and a little humid.
Because of this, culture techniques have inherent limitations.
Culture Limitations
Firstly, culture techniques only capture a fraction of the microbial diversity present in the gut.
Culture primarily focuses on bacteria that can survive aerobic conditions (meaning normal oxygen-rich air) than strict anaerobic bacteria (oxygen kills them). Anaerobic bacteria make up the vast majority of the gut microbiome.
Culture generally favours fast-growing bacteria, missing many slower-growing or fastidious (different growth requirement) species that play crucial roles in gut health.
Culture plates are often overgrown by certain species, either swarming bacteria like Proteus or by fast-growing E. coli. e.g., E. coli in a PCR-based microbiome test would typically represent between 0.1–1% of the microbiome. On an overgrown culture plate this can look like 80% or 4+ growth.
While culture can be useful in some circumstances, it doesn't accurately describe the complex community present within the gut microbiome, and results in a false representation of gut diversity.
In contrast, PCR offers a more comprehensive and accurate approach. It is a molecular biology technique meaning it amplifies specific DNA sequences from the microbial species present in your stool sample.
This allows for the detection and community profiling of a massive range of bacteria, fungi, and other microorganisms compared with culture.
PCR Advantages
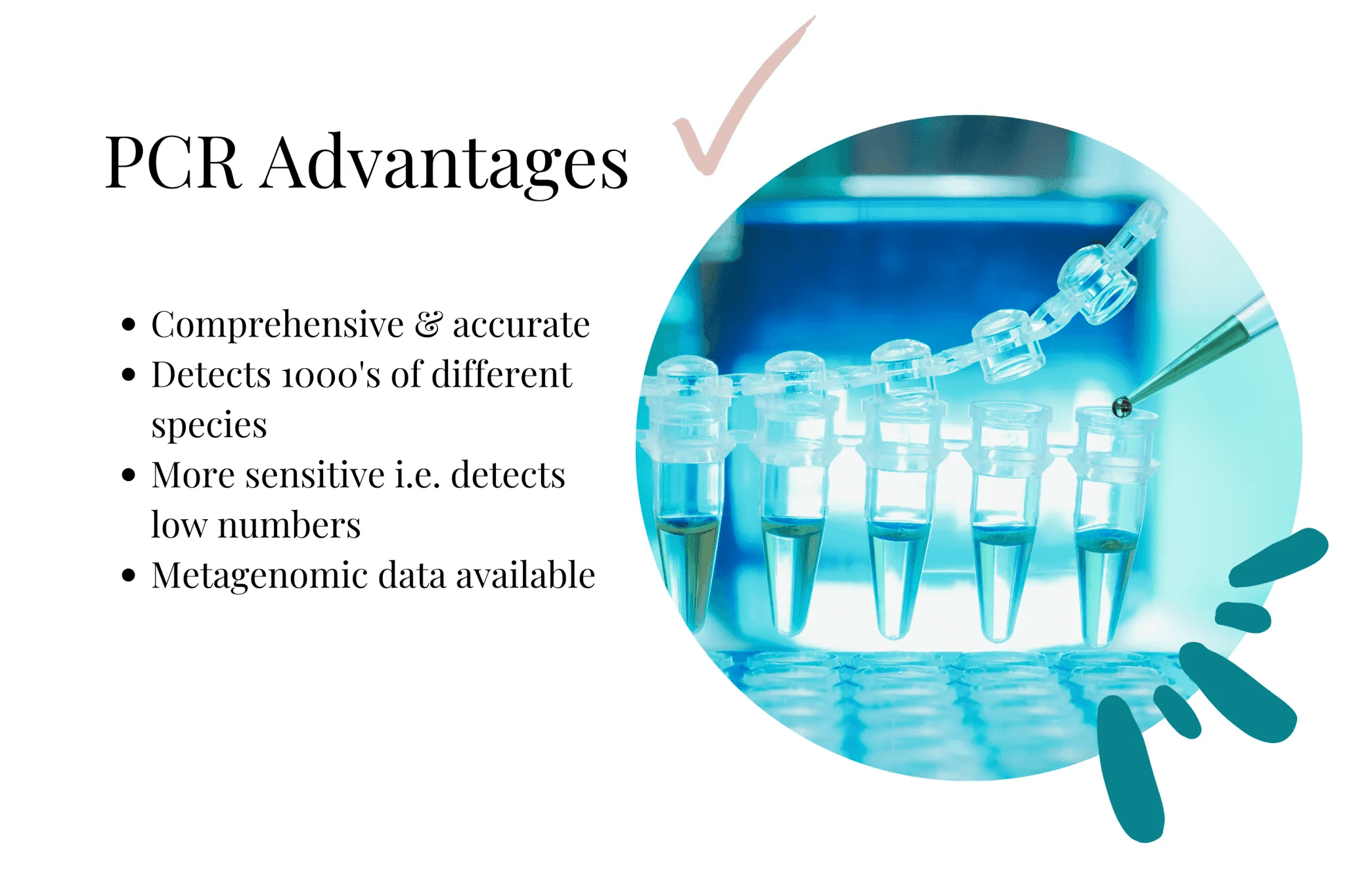
PCR is not limited by the need for bacterial growth in culture, making it ideal for capturing the true microbial diversity within each individual gut sample.
As a guide, typical PCR-based microbiome reports we receive describe, on average, between 200–800 bacterial species. The report lists every single species and strain of those 800-odd bacteria.
And many of these species account for as little as 0.003% of the microbiome.
We also see a typical high diversity profile averaging no more than 4–5% of the microbiome being represented by a single strain.
These results are very different than culture results which give relative quantities like 2+ and/or 'present' or 'absent'.
We can see and identify specific bacterial strains that need to be higher, and those that are taking over.
We also receive impact insights into metagenomic data—pathways in the body that bacterial genes represent. This includes Short Chain Fatty Acids (SCFAs), vitamin groups, harmful metabolites like lipopolysaccharide (LPS) and more.
In addition to the bacterial numbers, this information is invaluable for pinpointing deeper imbalances and guiding targeted interventions to restore gut health.
In the next section, we'll explore examples of advanced gut microbiome testing methods used in Australia, shedding light on the innovative approaches available for assessing gut health.
Examples of Gut Microbiome Testing Methods Used in Australia
In Australia, gut microbiome testing uses two prominent methods:
Advanced throughput sequencing, also known as next-generation sequencing (NGS), allows the simultaneous sequencing of millions of DNA fragments. Using advanced targeted bioinformatics techniques 16s rRNA gene-sequencing enables labs to very accurately identify and quantify gut microbial species present in a sample using known DNA fragments.
Shotgun metagenomic sequencing involves sequencing all DNA present in a sample, and provides a comprehensive snapshot of the entire community—including non-rRNA organisms like fungi. This method also investigates functional information from samples, such as the presence of antibiotic resistance genes and how species co-vary.
Both methods offer valuable insights into the gut microbiome, but they differ in their scope and applications. NGS provides high-resolution taxonomic data, making it ideal for studying microbial diversity and community composition.
On the other hand, shotgun metagenomic sequencing offers a wider view of the gut microbiome, including functional and genetic information.
How We Utilise Gut Microbiome Testing
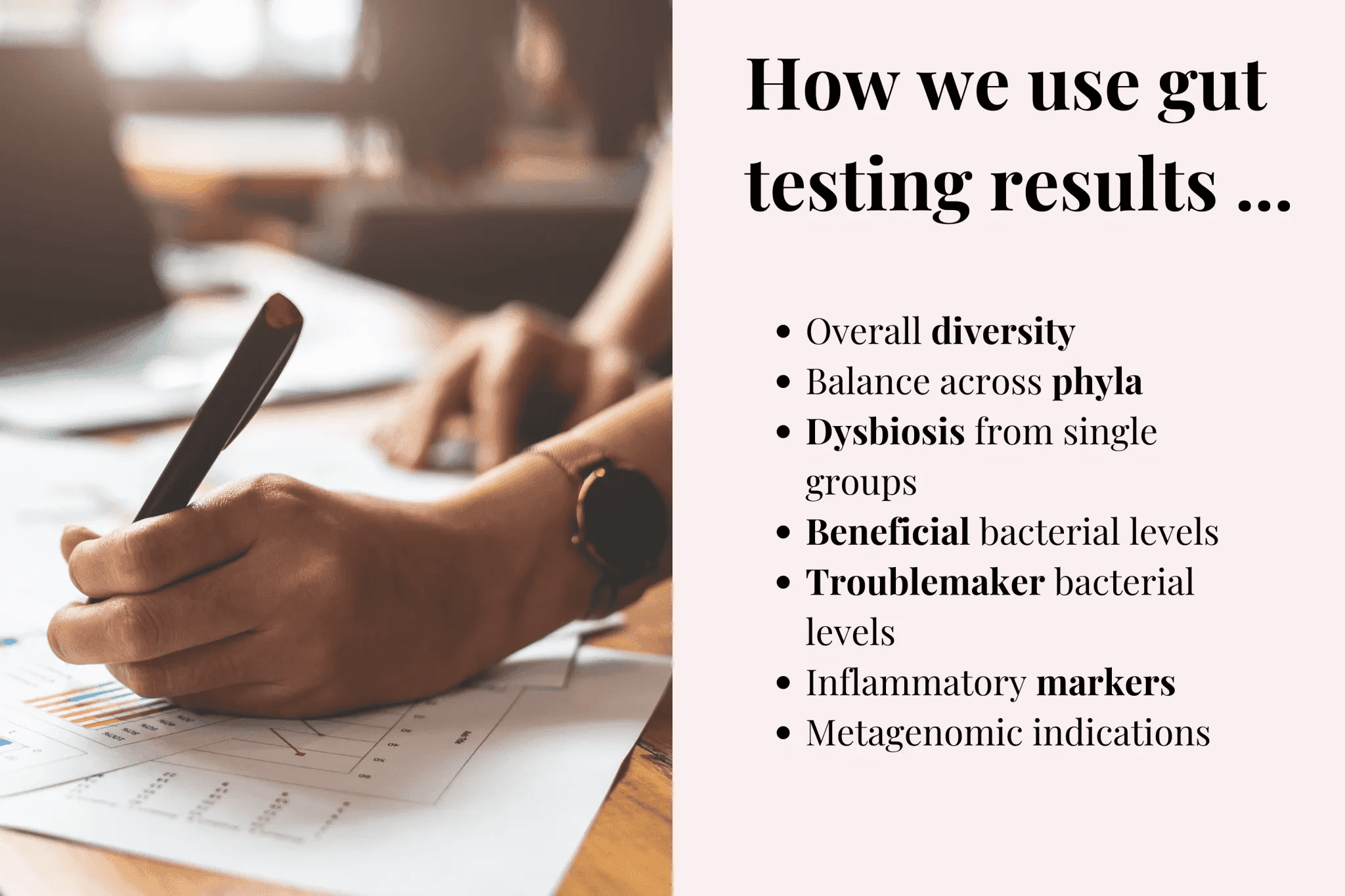
Every gut health program our team runs includes gut microbiome testing.
Rather than guess what's going on based on symptoms, we choose to find out exact numbers of the bacteria in your gut and target treatment plans accordingly.
We workshop every client report we receive, and go through the incredibly in-depth report, along with 2 supplementary reports.
There are a number of areas we look at when assessing a report:
Overall diversity
Balance across phyla (large microbiome groups)
Dysbiosis from single species or groups
Beneficial bacterial levels (like Akkermansia, Lactobacillus, Bifidobacterium…)
Troublemaker bacterial levels
Inflammatory markers
And many many more metagenomic markers provided
All this is taken into consideration with your symptoms and history to build an accurate picture of what is going on. A targeted plan is then developed with naturopathic principles along with diet and lifestyle recommendations indicated by your report.

